2024
Genetic Risk Factors for Early-Onset Merkel Cell Carcinoma
Mohsin, N., Hunt, D., Yan, J., Jabbour, A. J., Nghiem, P., Choi, J., Zhang, Y., Freeman, A. F., Bergerson, J. R. E., Dell'Orso, S., Lachance, K., Kulikauskas, R., Collado, L., Cao, W., Lack, J., Similuk, M., Seifert, B. A., Ghosh, R., Walkiewicz, M. A., & Brownell, I
JAMA dermatology, e235362. Advance online publication. https://doi.org/10.1001/jamadermatol.2023.5362
PMID: 38170500
Abstract and Highlights
- Importance: Merkel cell carcinoma (MCC) is a rare, aggressive neuroendocrine skin cancer. Of the patients who develop MCC annually, only 4% are younger than 50 years.
- Objective: To identify genetic risk factors for early-onset MCC via genomic sequencing.
- Design, setting, and participants: The study represents a multicenter collaboration between the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute of Allergy and Infectious Diseases (NIAID), and the University of Washington. Participants with early-onset and later-onset MCC were prospectively enrolled in an institutional review board-approved study at the University of Washington between January 2003 and May 2019. Unrelated controls were enrolled in the NIAID Centralized Sequencing Program (CSP) between September 2017 and September 2021. Analysis was performed from September 2021 and March 2023. Early-onset MCC was defined as disease occurrence in individuals younger than 50 years. Later-onset MCC was defined as disease occurrence at age 50 years or older. Unrelated controls were evaluated by the NIAID CSP for reasons other than familial cancer syndromes, including immunological, neurological, and psychiatric disorders.
- Results: This case-control analysis included 1012 participants: 37 with early-onset MCC, 45 with later-onset MCC, and 930 unrelated controls. Among 37 patients with early-onset MCC, 7 (19%) had well-described variants in genes associated with cancer predisposition. Six patients had variants associated with hereditary cancer syndromes (ATM = 2, BRCA1 = 2, BRCA2 = 1, and TP53 = 1) and 1 patient had a variant associated with immunodeficiency and lymphoma (MAGT1). Compared with 930 unrelated controls, the early-onset MCC cohort was significantly enriched for cancer-predisposing pathogenic or likely pathogenic variants in these 5 genes (odds ratio, 30.35; 95% CI, 8.89-106.30; P < .001). No germline disease variants in these genes were identified in 45 patients with later-onset MCC. Additional variants in DNA repair genes were also identified among patients with MCC.
- Conclusions and relevance: Because variants in certain DNA repair and cancer predisposition genes are associated with early-onset MCC, genetic counseling and testing should be considered for patients presenting at younger than 50 years.
2023
Enhancing immunogenic responses through CDK4/6 and HIF2α inhibition in Merkel cell carcinoma
Lee, J. H., Lee, J. D., Paulson, K., Voillet, V., Berndt, A., Church, C., Lachance, K., Park, S. Y., Yamamoto, N. K., Cromwell, E. A., Gottardo, R., Chapuis, A. G., & Nghiem, P
Heliyon, 10(1), e23521. https://doi.org/10.1016/j.heliyon.2023.e23521
PMID: 38173534
Abstract and Highlights
- Approximately 50% of Merkel cell carcinoma (MCC) patients facing this highly aggressive skin cancer initially respond positively to PD-1-based immunotherapy. Nevertheless, the recurrence of MCC post-immunotherapy emphasizes the pressing need for more effective treatments. Recent research has highlighted Cyclin-dependent kinases 4 and 6 (CDK4/6) as pivotal cell cycle regulators gaining prominence in cancer studies. This study reveals that the CDK4/6 inhibitor, palbociclib can enhance PD-L1 gene transcription and surface expression in MCC cells by activating HIF2α. Inhibiting HIF2α with TC-S7009 effectively counteracts palbociclib-induced PD-L1 transcription and significantly intensifies cell death in MCC. Simultaneously, co-targeting CDK4/6 and HIF2α boosts ROS levels while suppressing SLC7A11, a key regulator of cellular redox balance, promoting ferroptosis- a form of immunogenic cell death linked to iron. Considering the rising importance of immunogenic cell death in immunotherapy, this strategy holds promise for improving future MCC treatments, markedly increasing immunogenic cell death various across various MCC cell lines, thus advancing cancer immunotherapy.
Merkel cell carcinoma recurrence risk estimation is improved by integrating factors beyond cancer stage: A multivariable model and web-based calculator
McEvoy, A. M., Hippe, D. S., Lachance, K., Park, S., Cahill, K., Redman, M., Gooley, T., Kattan, M. W., & Nghiem, P
Journal of the American Academy of Dermatology, S0190-9622(23)03220-6. Advance online publication. https://doi.org/10.1016/j.jaad.2023.11.020
PMID: 37984720
Abstract and Highlights
- Background: Merkel cell carcinoma (MCC) recurs in 40% of patients. In addition to stage, factors known to affect recurrence risk include: sex, immunosuppression, unknown primary status, age, site of primary tumor, and time since diagnosis.
- Purpose: Create a multivariable model and web-based calculator to predict MCC recurrence risk more accurately than stage alone.
- Methods: Data from 618 patients in a prospective cohort were used in a competing risk regression model to estimate recurrence risk using stage and other factors.
- Results: In this multivariable model, the most impactful recurrence risk factors were: American Joint Committee on Cancer stage (P < .001), immunosuppression (hazard ratio 2.05; P < .001), male sex (1.59; P = .003) and unknown primary (0.65; P = .064). Compared to stage alone, the model improved prognostic accuracy (concordance index for 2-year risk, 0.66 vs 0.70; P < .001), and modified estimated recurrence risk by up to 4-fold (18% for low-risk stage IIIA vs 78% for high-risk IIIA over 5 years).
- Limitations: Lack of an external data set for model validation.
- Conclusion/relevance: As demonstrated by this multivariable model, accurate recurrence risk prediction requires integration of factors beyond stage. An online calculator based on this model (at merkelcell.org/recur) integrates time since diagnosis and provides new data for optimizing surveillance for MCC patients.
Extended duration of treatment using reduced-frequency dosing of anti-PD-1 therapy in patients with advanced melanoma and Merkel cell carcinoma
Tachiki, L. M. L., Hippe, D. S., Williams Silva, K., Hall, E. T., McCamy, W., Fritzsche, D., Perdue, A., Majovski, J., Pulliam, T., Goldstein, D. A., Veatch, J., Ho, J., Nghiem, P. T., Thompson, J. A., & Bhatia, S
Cancer immunology, immunotherapy : CII, 72(11), 3839–3850. https://doi.org/10.1007/s00262-023-03539-8
PMID: 37733060
Abstract and Highlights
- Background: Optimal duration of treatment (DoT) with immune checkpoint inhibitors (ICI) in metastatic cancers remains unclear. Many patients, especially those without radiologic complete remission, develop progressive disease after ICI discontinuation. Extending DoT with ICI may potentially improve efficacy outcomes but presents major logistical and cost challenges with standard frequency dosing (SFD). Receptor occupancy data supports reduced frequency dosing (RFD) of anti-PD-1 antibodies, which may represent a more practical and economically viable option to extend DoT.
- Methods: We conducted a retrospective study of patients with metastatic melanoma and Merkel cell carcinoma (MCC), who received ICI at RFD administered every 3 months, after initial disease control at SFD. We evaluated efficacy, safety, and cost-savings of the RFD approach in this cohort.
- Results: Between 2014 and 2021, 23 patients with advanced melanoma (N = 18) or MCC (N = 5) received anti-PD-1 therapy at RFD. Median DoT was 1.1 years at SFD and 1.2 years at RFD. The 3 year PFS after start of RFD was 73% in melanoma and 100% in MCC patients, which compare favorably to historical control rates. In the subset of 15 patients who received at least 2 years of therapy, total savings amounted to $1.1 million in drug costs and 384 h saved despite the extended DoT (median 3.4 years), as compared to the calculated cost of 2 years at SFD.
- Conclusions: ICI administration at RFD can allow extension of treatment duration, while preserving efficacy and reducing logistical and financial burden. RFD approach deserves further exploration in prospective clinical trials.
Characterization of immunosuppressive myeloid cells in Merkel cell carcinoma: correlation with resistance to PD-1 pathway blockade
Tabachnick-Cherny, S., Pulliam, T., Rodriguez, H. J., Fan, X., Hippe, D. S., Jones, D. C., Moshiri, A. S., Smythe, K. S., Kulikauskas, R. M., Zaba, L., Paulson, K. G., & Nghiem, P
Clinical cancer research : an official journal of the American Association for Cancer Research, 10.1158/1078-0432.CCR-23-1957. Advance online publication. https://doi.org/10.1158/1078-0432.CCR-23-1957
PMID: 37851052
Abstract and Highlights
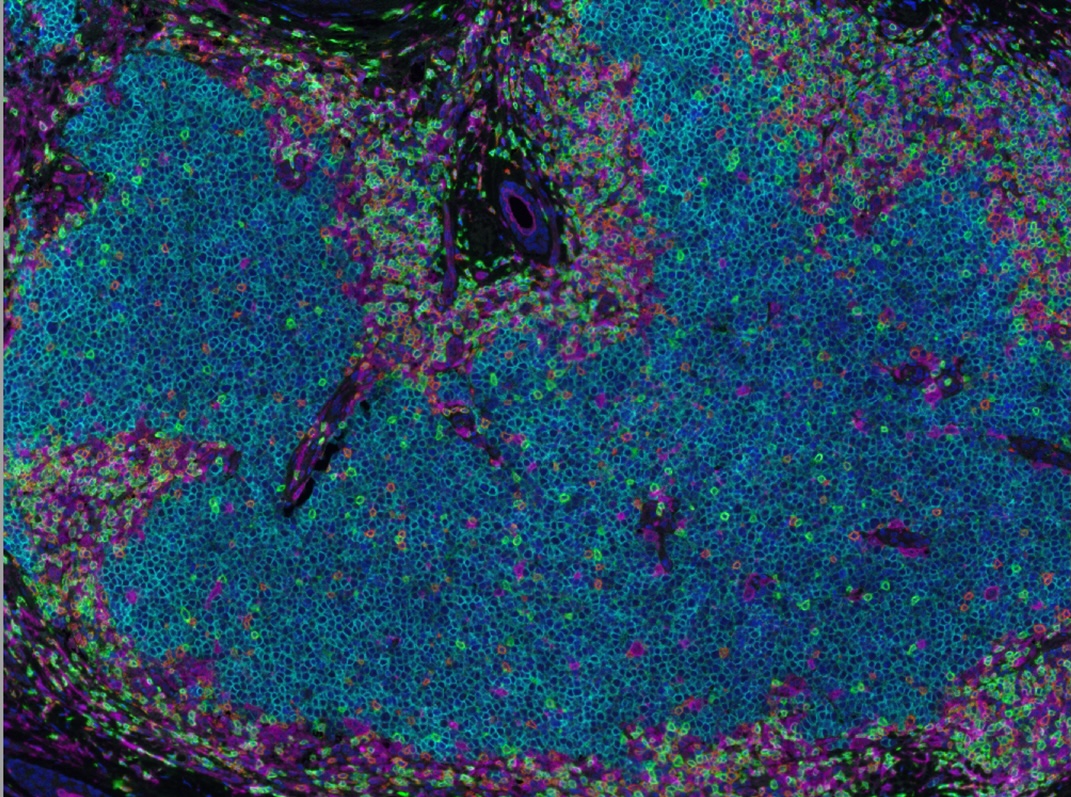
- Purpose: Merkel cell carcinoma (MCC) is a highly immunogenic skin cancer. Although essentially all MCCs are antigenic through viral antigens or high tumor mutation burden, MCC has a response rate of only ~50% to PD-(L)1 blockade suggesting barriers to T cell responses. Prior studies of MCC immunobiology have focused on CD8 T-cell infiltration and their exhaustion status, while the role of innate immunity, particularly myeloid cells, in MCC remains underexplored.
- Experimental design: We utilized single cell transcriptomics from 9 MCC patients and multiplex-immunohistochemistry staining of 54 patients’ pre-immunotherapy tumors, to identify myeloid cells and evaluate association with immunotherapy response.
- Results: Single cell transcriptomics identified tumor-associated macrophages (TAMs) as the dominant myeloid component within MCC tumors. These TAMs express an immunosuppressive gene signature characteristic of monocytic myeloid derived suppressor cells and importantly express several targetable immune checkpoint molecules, including PD-L1 and LILRB receptors, that are not present on tumor cells. Analysis of 54 pre-immunotherapy tumor samples showed that a subset of TAMs (CD163+, CD14+, S100A8+) selectively infiltrated tumors that had significant CD8 T-cells. Indeed, higher TAM prevalence was associated with resistance to PD-1 blockade. While spatial interactions between TAMs and CD8 T cells were not associated with response, myeloid transcriptomic data showed evidence for cytokine signaling and expression of LILRB receptors, suggesting potential immunosuppressive mechanisms.
- Conclusions: This study further characterizes TAMs in MCC tumors and provides insights into their possible immunosuppressive mechanism. TAMs may reduce the likelihood of treatment response in MCC by counteracting the benefit of CD8 T-cell infiltration.
Increased risk of recurrence and disease-specific death following delayed postoperative radiation for Merkel cell carcinoma
Alexander, N. A., Schaub, S. K., Goff, P. H., Hippe, D. S., Park, S. Y., Lachance, K., Bierma, M., Liao, J. J., Apisarnthanarax, S., Bhatia, S., Tseng, Y. D., Nghiem, P. T., & Parvathaneni, U
Journal of the American Academy of Dermatology, 90(2), 261–268. https://doi.org/10.1016/j.jaad.2023.07.1047
PMID: 37778663
Abstract and Highlights
- Background: Merkel cell carcinoma (MCC) is often treated with surgery and postoperative radiation therapy (PORT). The optimal time to initiate PORT (Time-to-PORT [ttPORT]) is unknown.
- Purpose: We assessed if delays in ttPORT were associated with inferior outcomes.
- Methods: Competing risk regression was used to evaluate associations between ttPORT and locoregional recurrence (LRR) for patients with stage I/II MCC in a prospective registry and adjust for covariates. Distant metastasis and death were competing risks.
- Results: The cohort included 124 patients with median ttPORT of 41 days (range: 8-125 days). Median follow-up was 55 months. 17 (14%) patients experienced a LRR, 14 (82%) of which arose outside the radiation field. LRR at 5 years was increased for ttPORT >8 weeks vs ≤ 8 weeks, 28.0% vs 9.2%, P = .006. There was an increase in the cumulative incidence of MCC-specific death with increasing ttPORT (HR = 1.14 per 1-week increase, P = .016).
- Limitations: The relatively low number of LRRs limited the extent of our multivariable analyses.
- Conclusions: Delay of PORT was associated with increased LRR, usually beyond the radiation field. This is consistent with the tendency of MCC to spread quickly via lymphatics. Initiation of PORT within 8 weeks was associated with improved locoregional control and MCC-specific survival.
LAMP1 targeting of the large T antigen of Merkel cell polyomavirus results in potent CD4 T cell responses and tumor inhibition
Buchta Rosean, C., Leyder, E. C., Hamilton, J., Carter, J. J., Galloway, D. A., Koelle, D. M., Nghiem, P., & Heiland, T
Frontiers in immunology, 14, 1253568. https://doi.org/10.3389/fimmu.2023.1253568
PMID: 37711623
- Introduction: Most cases of Merkel cell carcinoma (MCC), a rare and highly aggressive type of neuroendocrine skin cancer, are associated with Merkel cell polyomavirus (MCPyV) infection. MCPyV integrates into the host genome, resulting in expression of oncoproteins including a truncated form of the viral large T antigen (LT) in infected cells. These oncoproteins are an attractive target for a therapeutic cancer vaccine.
- Methods: We designed a cancer vaccine that promotes potent, antigen-specific CD4 T cell responses to MCPyV-LT. To activate antigen-specific CD4 T cells in vivo, we utilized our nucleic acid platform, UNITE™ (UNiversal Intracellular Targeted Expression), which fuses a tumor-associated antigen with lysosomal-associated membrane protein 1 (LAMP1). This lysosomal targeting technology results in enhanced antigen presentation and potent antigen-specific T cell responses. LTS220A, encoding a mutated form of MCPyV-LT that diminishes its pro-oncogenic properties, was introduced into the UNITE™ platform.
- Results: Vaccination with LTS220A-UNITE™ DNA vaccine (ITI-3000) induced antigen-specific CD4 T cell responses and a strong humoral response that were sufficient to delay tumor growth of a B16F10 melanoma line expressing LTS220A. This effect was dependent on the CD4 T cells’ ability to produce IFNγ. Moreover, ITI-3000 induced a favorable tumor microenvironment (TME), including Th1-type cytokines and significantly enhanced numbers of CD4 and CD8 T cells as well as NK and NKT cells. Additionally, ITI-3000 synergized with an α-PD-1 immune checkpoint inhibitor to further slow tumor growth and enhance survival.
- Conclusions: These findings strongly suggest that in pre-clinical studies, DNA vaccination with ITI-3000, using the UNITE™ platform, enhances CD4 T cell responses to MCPyV-LT that result in significant anti-tumor immune responses. These data support the initiation of a first-in-human (FIH) Phase 1 open-label study to evaluate the safety, tolerability, and immunogenicity of ITI-3000 in patients with polyomavirus-positive MCC (NCT05422781).
Postoperative Radiation Therapy Is Indicated for “Low-Risk” Pathologic Stage I Merkel Cell Carcinoma of the Head and Neck Region but Not for Other Locations
Bierma, M. M., Goff, P. H., Hippe, D. S., Lachance, K., Schaub, S. K., Wallner, K., Tseng, Y. D., Liao, J. J., Apisarnthanarax, S., Nghiem, P., & Parvathaneni, U
Advances in radiation oncology, 9(2), 101364. https://doi.org/10.1016/j.adro.2023.101364
PMID: 38189056
Abstract and Highlights
- Purpose: The role of postoperative radiation therapy (PORT) in early stage Merkel cell carcinoma (MCC) is controversial. We analyzed the role of PORT in preventing local recurrences (LR) among patients with low-risk, pathologic stage I MCC based on the location of the primary tumors: head/neck (HN) versus non-HN sites.
- Methods and materials: One hundred forty-seven patients with MCC were identified that had “low risk” disease (pathologic T1 primary tumor, negative microscopic margins, negative pathologic node status, no immunosuppression or prior systemic therapy). LR was defined as tumor recurrence within 2 cm of the primary surgical bed, and its frequency was estimated with the cumulative incidence method.
- Results: Seventy-nine patients received PORT (30 HN, 49 non-HN) with a median dose of 50 Gy (range, 8-64 Gy) and 68 patients were treated with surgery alone (30 HN, 38 non-HN). Overall, PORT was associated with a decreased risk of LR (5-year rate: 0% vs 9.5%; P = .004) with 6 LRs observed in the surgery alone group. Although the addition of PORT significantly reduced LR rates among patients with HN MCC (0% vs. 21%; P = .034), no LRs were observed in patients with non-HN MCC managed with surgery alone. There was no significant difference in MCC-specific survival comparing HN versus non-HN groups, with or without PORT.
- Conclusions: For low-risk, pathologic stage I MCC of the extremities and trunk, excellent local control rates were achieved with surgery, and PORT is not indicated. However, PORT was associated with a significant reduction in LRs among low-risk MCC of the HN.
The Evolving Treatment Landscape of Merkel Cell Carcinoma
Singh, N., McClure, E. M., Akaike, T., Park, S. Y., Huynh, E. T., Goff, P. H., & Nghiem, P
Curr Treat Options Oncol. 2023 Jul 5. doi: 10.1007/s11864-023-01118-8. Online ahead of print.
PMID: 37403007
Abstract and Highlights
- Our team based in Seattle conducted a comprehensive review including evolving trends in the management of Merkel cell carcinoma (MCC). This summary covers key decision points, including recommended work-up during initial diagnosis, treatment options for MCC when it’s in one place or has spread, management of recurrent MCC, and new treatments that are showing promise with fewer side effects and good results. This review gives valuable information on how to handle MCC overall and emphasizes new methods that are effective and less toxic on patients.
- Merkel cell carcinoma (MCC) has a high risk of recurrence and requires unique treatment relative to other skin cancers. The patient population is generally older, with comorbidities. Multidisciplinary and personalized care is therefore paramount, based on patient preferences regarding risks and benefits. Positron emission tomography and computed tomography (PET-CT) is the most sensitive staging modality and reveals clinically occult disease in ~ 16% of patients. Discovery of occult disease spread markedly alters management. Newly diagnosed, localized disease is often managed with sentinel lymph node biopsy (SLNB), local excision, primary wound closure, and post-operative radiation therapy (PORT). In contrast, metastatic disease is usually treated systemically with an immune checkpoint inhibitor (ICI). However, one or more of these approaches may not be indicated. Criteria for such exceptions and alternative approaches will be discussed. Because MCC recurs in 40% of patients and early detection/treatment of advanced disease is advantageous, close surveillance is recommended. Given that over 90% of initial recurrences arise within 3 years, surveillance frequency can be rapidly decreased after this high-risk period. Patient-specific assessment of risk is important because recurrence risk varies widely (15 to > 80%: Merkelcell.org/recur) depending on baseline patient characteristics and time since treatment. Blood-based surveillance tests are now available (Merkel cell polyomavirus (MCPyV) antibodies and circulating tumor DNA (ctDNA)) with excellent sensitivity that can spare patients from contrast dye, radioactivity, and travel to a cancer imaging facility. If recurrent disease is locoregional, management with surgery and/or RT is typically indicated. ICIs are now the first line for systemic/advanced MCC, with objective response rates (ORRs) exceeding 50%. Cytotoxic chemotherapy is sometimes used for debulking disease or in patients who cannot tolerate ICI. ICI-refractory disease is the major problem faced by this field. Fortunately, numerous promising therapies are on the horizon to address this clinical need.
Insights into anti-tumor immunity via the polyomavirus shared across human Merkel cell carcinomas
Jani, S., Church, C. D., & Nghiem, P
Front Immunol. 2023 May 23;14:1172913. doi: 10.3389/fimmu.2023.1172913. eCollection 2023.
PMID: 37287968
Abstract and Highlights
- Understanding and augmenting cancer-specific immunity is impeded by the fact that most tumors are driven by patient-specific mutations that encode unique antigenic epitopes. The shared antigens in virus-driven tumors can help overcome this limitation. Merkel cell carcinoma (MCC) is a particularly interesting tumor immunity model because (1) 80% of cases are driven by Merkel cell polyomavirus (MCPyV) oncoproteins that must be continually expressed for tumor survival; (2) MCPyV oncoproteins are only ~400 amino acids in length and are essentially invariant between tumors; (3) MCPyV-specific T cell responses are robust and strongly linked to patient outcomes; (4) anti-MCPyV antibodies reliably increase with MCC recurrence, forming the basis of a standard clinical surveillance test; and (5) MCC has one of the highest response rates to PD-1 pathway blockade among all solid cancers. Leveraging these well-defined viral oncoproteins, a set of tools that includes over 20 peptide-MHC class I tetramers has been developed to facilitate the study of anti-tumor immunity across MCC patients. Additionally, the highly immunogenic nature of MCPyV oncoproteins forces MCC tumors to develop robust immune evasion mechanisms to survive. Indeed, several immune evasion mechanisms are active in MCC, including transcriptional downregulation of MHC expression by tumor cells and upregulation of inhibitory molecules including PD-L1 and immunosuppressive cytokines. About half of patients with advanced MCC do not persistently benefit from PD-1 pathway blockade. Herein, we (1) summarize the lessons learned from studying the anti-tumor T cell response to virus-positive MCC; (2) review immune evasion mechanisms in MCC; (3) review mechanisms of resistance to immune-based therapies in MCC and other cancers; and (4) discuss how recently developed tools can be used to address open questions in cancer immunotherapy. We believe detailed investigation of this model cancer will provide insight into tumor immunity that will likely also be applicable to more common cancers without shared tumor antigens.
2022
Management and Prognosis of Cardiac Metastatic Merkel Cell Carcinoma: A Case–Control Study and Literature Review
Akaike T, Cahill K, Akaike G, Huynh ET, Hippe DS, Shinohara MM, Liao J, Apisarnthanarax S, Parvathaneni U, Hall E, Bhatia S, Cheng RK, Nghiem P, Tseng YD
PMID: 36497395
Abstract and Highlights
- This case study looks at 9 patients who developed cardiac metastases, a tricky situation on which very little data is currently available. We hope that by describing 9 cases, this will provide an easily accessible road map for clinicians around the world when this difficult situation arises. In many cases, the combination of limited ‘palliative’ radiation with immune therapy proved beneficial.
- Merkel cell carcinoma (MCC), an aggressive neuroendocrine skin cancer, has a high rate (20%) of distant metastasis. Within a prospective registry of 582 patients with metastatic MCC (mMCC) diagnosed between 2003–2021, we identified 9 (1.5%) patients who developed cardiac metastatic MCC (mMCC). We compared overall survival (OS) between patients with cardiac and non-cardiac metastases in a matched case–control study. Cardiac metastasis was a late event (median 925 days from initial MCC diagnosis). The right heart was predominantly involved (8 of 9; 89%). Among 7 patients treated with immunotherapy, 6 achieved a complete or partial response of the cardiac lesion. Among these 6 responders, 5 received concurrent cardiac radiotherapy (median 20 Gray) with immunotherapy; 4 of 5 did not have local disease progression or recurrence in the treated cardiac lesion. One-year OS was 44%, which was not significantly different from non-cardiac mMCC patients (45%, p = 0.96). Though it occurs relatively late in the disease course, cardiac mMCC responded to immunotherapy and/or radiotherapy and was not associated with worse prognosis compared to mMCC at other anatomic sites. These results are timely as cardiac mMCC may be increasingly encountered in the era of immunotherapy as patients with metastatic MCC live longer.
Transcriptional and functional analyses of neoantigen-specific CD4 T cells during a profound response to anti-PD-L1 in metastatic Merkel cell carcinoma
Church C, Pulliam T, Longino N, Park SY, Smythe KS, Makarov V, Riaz N, Jing L, Amezquita R, Campbell JS, Gottardo R, Pierce RH, Choi J, Chan T, Koelle DM, Nghiem P
Abstract and Highlights
- Background Merkel cell carcinoma (MCC) often responds to PD-1 pathway blockade, regardless of tumor-viral status (~80% of cases driven by the Merkel cell polyomavirus (MCPyV)). Prior studies have characterized tumor-specific T cell responses to MCPyV, which have typically been CD8, but little is known about the T cell response to UV-induced neoantigens.
- Methods A patient in her mid-50s with virus-negative (VN) MCC developed large liver metastases after a brief initial response to chemotherapy. She received anti-PD-L1 (avelumab) and had a partial response within 4 weeks. Whole exome sequencing (WES) was performed to determine potential neoantigen peptides. Characterization of peripheral blood neoantigen T cell responses was evaluated via interferon-gamma (IFNγ) ELISpot, flow cytometry and single-cell RNA sequencing. Tumor-resident T cells were characterized by multiplexed immunohistochemistry.
- Results WES identified 1027 tumor-specific somatic mutations, similar to the published average of 1121 for VN-MCCs. Peptide prediction with a binding cut-off of ≤100 nM resulted in 77 peptides that were synthesized for T cell assays. Although peptides were predicted based on class I HLAs, we identified circulating CD4 T cells targeting 5 of 77 neoantigens. In contrast, no neoantigen-specific CD8 T cell responses were detected. Neoantigen-specific CD4 T cells were undetectable in blood before anti-PD-L1 therapy but became readily detectible shortly after starting therapy. T cells produced robust IFNγ when stimulated by neoantigen (mutant) peptides but not by the normal (wild-type) peptides. Single cell RNAseq showed neoantigen-reactive T cells expressed the Th1-associated transcription factor (T-bet) and associated cytokines. These CD4 T cells did not significantly exhibit cytotoxicity or non-Th1 markers. Within the pretreatment tumor, resident CD4 T cells were also Th1-skewed and expressed T-bet.
- Conclusions We identified and characterized tumor-specific Th1-skewed CD4 T cells targeting multiple neoantigens in a patient who experienced a profound and durable partial response to anti-PD-L1 therapy. To our knowledge, this is the first report of neoantigen-specific T cell responses in MCC. Although CD4 and CD8 T cells recognizing viral tumor antigens are often detectible in virus-positive MCC, only CD4 T cells recognizing neoantigens were detected in this patient. These findings suggest that CD4 T cells can play an important role in the response to anti-PD-(L)1 therapy.
Real-world clinical outcomes with avelumab in patients with Merkel cell carcinoma treated in the United States: a multicenter chart review study
171. Bhatia S, Nghiem P, Veeranki SP, Vanegas A, Lachance K, Tachiki L, Chiu K, Boller E, Murtuza Bharmal M
J Immunother Cancer. 2022 Aug;10(8):e004904.
PMID: 35981787
Abstract and Highlights
- Background: Merkel cell carcinoma (MCC) is a rare, aggressive, cutaneous neuroendocrine neoplasm with annual incidence rates of 0.13-1.6 cases/100,000/year worldwide as of 2018. Chemotherapy for metastatic MCC (mMCC) has high objective response rates (ORRs), but responses are not durable and overall survival (OS) is poor. Avelumab (anti-programmed death-ligand 1) has demonstrated meaningful survival benefit and durable responses in clinical trials for mMCC. This study investigated real-world clinical outcomes in avelumab-treated patients with advanced (stage IIIB/IV) MCC in US academic medical centers.
- Methods: We conducted a retrospective chart review of patients with advanced MCC who initiated avelumab between March 1, 2017, and July 31, 2019, at six US academic centers. Data were requested for eligible patients from index date through December 31, 2020. Descriptive analyses were conducted to assess demographic and clinical characteristics, real-world ORR (rwORR), real-world duration of response, real-world progression-free survival (rwPFS), and OS.
- Results: Ninety patients with advanced MCC (82%, stage IV; 18%, stage IIIB) received avelumab. Median follow-up was 20.8 months (95% CI: 19.1 to 24.2). Median age was 68 years (range, 48-83), and the majority of patients were men (58%) and white (93%). The primary tumor was most commonly located on the lower limb (38%), with metastases mostly located in lymph nodes (68%), lung (52%), and viscera (52%). Approximately 42% and 26% of patients had an Eastern Cooperative Oncology Group performance status of 2 and 3, respectively. Seventy-three patients (81%) received avelumab as first-line treatment of advanced MCC, while 17 (19%) received avelumab as second-line or later treatment. The median duration of avelumab treatment was 13.5 months (95% CI: 6.4 to 30.6), with 42% of patients still receiving avelumab by the end of follow-up. Patients with avelumab treatment had an rwORR of 73% (95% CI: 64 to 83), median rwPFS of 24.4 months (95% CI: 8.31 to not estimable (NE)), and median OS of 30.7 months (95% CI: 11.2 to NE).
- Conclusions: This real-world study of patients with advanced MCC demonstrated that avelumab treatment resulted in a high response rate with durable responses and prolonged survival. The study findings validate the results demonstrated in prospective clinical trials and other observational studies.
Society for Immunotherapy of Cancer (SITC) clinical practice guideline on immunotherapy for the treatment of nonmelanoma skin cancer
Silk AW, Barker CA, Bhatia S, Bollin KB, Chandra S, Eroglu Z, Gastman BR, Kendra KL, Kluger H, Lipson EJ, Madden K, Miller DM, Nghiem P, Pavlick AC, Puzanov I, Rabinowits G, Ruiz ES, Sondak VK, Tavss EA, Tetzlaff MT, Brownell I
J Immunother Cancer. 2022 Jul;10(7):e004434. doi: 10.1136/jitc-2021-004434.
PMID: 35902131
Abstract and Highlights
- Nonmelanoma skin cancers (NMSCs) are some of the most commonly diagnosed malignancies. In general, early-stage NMSCs have favorable outcomes; however, a small subset of patients develop resistant, advanced, or metastatic disease, or aggressive subtypes that are more challenging to treat successfully. Recently, immune checkpoint inhibitors (ICIs) have been approved by the US Food and Drug Administration (FDA) for the treatment of Merkel cell carcinoma (MCC), cutaneous squamous cell carcinoma (CSCC), and basal cell carcinoma (BCC). Although ICIs have demonstrated activity against NMSCs, the routine clinical use of these agents may be more challenging due to a number of factors including the lack of predictive biomarkers, the need to consider special patient populations, the management of toxicity, and the assessment of atypical responses. With the goal of improving patient care by providing expert guidance to the oncology community, the Society for Immunotherapy of Cancer (SITC) convened a multidisciplinary panel of experts to develop a clinical practice guideline (CPG). The expert panel drew on the published literature as well as their own clinical experience to develop recommendations for healthcare professionals on important aspects of immunotherapeutic treatment for NMSCs, including staging, biomarker testing, patient selection, therapy selection, post-treatment response evaluation and surveillance, and patient quality of life (QOL) considerations, among others. The evidence- and consensus-based recommendations in this CPG are intended to provide guidance to cancer care professionals treating patients with NMSCs.
Assessment of hyperprogression versus the natural course of disease development with nivolumab with or without ipilimumab versus placebo in phase III, randomized, controlled trials
Kang YK, Reck M, Nghiem P, Feng Y, Plautz G, Kim HR, Owonikoko TK, Boku N, Chen LT, Lei M, Chang H, Lin WH, Roy A, Bello A, Sheng J
J Immunother Cancer. 2022 Apr;10(4):e004273. doi: 10.1136/jitc-2021-004273
PMID: 35383114
Abstract and Highlights
- Background: Retrospective studies have suggested a potential risk of hyperprogressive disease (HPD) in patients receiving immune checkpoint inhibitors (ICIs). We compared the incidence of HPD during treatment with nivolumab±ipilimumab versus natural tumor progression with placebo in post hoc analyses of two randomized, double-blind clinical trials.
- Methods: ATTRACTION-2 randomized patients with advanced gastric or gastroesophageal junction cancer (GC/GEJC) and progression on ≥2 prior regimens to nivolumab 3 mg/kg Q2W or placebo. CheckMate 451 randomized patients with extensive-disease small cell lung cancer (ED SCLC) and ongoing complete/partial response or stable disease after first-line chemotherapy to nivolumab 240 mg Q2W, nivolumab 1 mg/kg+ipilimumab 3 mg/kg Q3W for four doses then nivolumab 240 mg Q2W, or placebo. Patients receiving ≥1 dose of study drug and with tumor scans at baseline and the first on-treatment evaluation were included in the HPD analyses. HPD definitions were ≥20%, ≥50%, and ≥100% increase in target lesion sum of the longest diameters (SLD) at the first on-treatment assessment.
- Results: In the ATTRACTION-2 HPD-evaluable population, 243 patients received nivolumab and 115 placebo. Fewer patients receiving nivolumab versus placebo had increases in SLD ≥20% (33.7% vs 46.1%) and ≥50% (6.2% vs 11.3%); similar proportions had increases in SLD ≥100% (1.6% vs 1.7%). In the CheckMate 451 HPD-evaluable population, 177 patients received nivolumab, 179 nivolumab+ipilimumab, and 175 placebo. Fewer patients receiving nivolumab or nivolumab+ipilimumab versus placebo had increases in SLD ≥20% (27.1%, 27.4% vs 45.7%), ≥50% (10.2%, 11.2% vs 22.3%), and ≥100% (2.8%, 2.8% vs 6.3%).
- Conclusions: Nivolumab±ipilimumab was not associated with an increased rate of progression versus placebo in patients with GC, GEJC, or ED SCLC, suggesting that previous reports of HPD may reflect the natural disease course in some patients rather than ICI-mediated progression.
Recurrence and Mortality Risk of Merkel Cell Carcinoma by Cancer Stage and Time From Diagnosis
McEvoy AM, Lachance K, Hippe DS, Cahill K, Moshiri Y, Lewis CW, Singh N, Park SY, Thuesmunn Z, Cook MM, Alexander N, Zawacki L, Thomas H, Paulson KG, Nghiem P.
JAMA Dermatol. 2022 Feb 23;e216096. doi: 10.1001/jamadermatol.2021.6096.
PMID: 35195657
Abstract and Highlights
- Importance: Merkel cell carcinoma (MCC) often behaves aggressively; however, disease-recurrence data are not captured in national databases, and it is unclear what proportion of patients with MCC experience a recurrence (estimates vary from 27%-77%). Stage-specific recurrence data that includes time from diagnosis would provide more precise prognostic information and contribute to risk-appropriate clinical surveillance.
- Objective: To estimate risk of stage-specific MCC recurrence and mortality over time since diagnosis.
- Design, setting, and participants: This prospective cohort study included 618 patients with MCC who were prospectively enrolled in a Seattle-based data repository between 2003 and 2019. Of these patients, 223 experienced a recurrence of MCC. Data analysis was performed July 2019 to November 2021.
- Main outcomes and measures: Stage-specific recurrence and survival, as well as cumulative incidence and Kaplan-Meier analyses.
- Results: Among the 618 patients included in the analysis (median [range] age, 69 [11-98] years; 227 [37%] female), the 5-year recurrence rate for MCC was 40%. Risk of recurrence in the first year was high (11% for patients with pathologic stage I, 33% for pathologic stage IIA/IIB, 30% for pathologic stage IIIA, 45% for pathologic stage IIIB, and 58% for pathologic stage IV), with 95% of recurrences occurring within the first 3 years. Median follow-up among living patients was 4.3 years. Beyond stage, 4 factors were associated with increased recurrence risk in univariable analyses: immunosuppression (hazard ratio [HR], 2.4; 95% CI, 1.7-3.3; P < .001), male sex (HR, 1.9; 95% CI, 1.4-2.5; P < .001), known primary lesion among patients with clinically detectable nodal disease (HR, 2.3; 95% CI, 1.4-4.0; P = .001), and older age (HR, 1.1; 95% CI, 1.0-1.3; P = .06 for each 10-year increase). Among 187 deaths in the cohort, 121 (65%) were due to MCC. The MCC-specific survival rate was strongly stage dependent (95% at 5 years for patients with pathologic stage I vs 41% for pathologic stage IV). Among patients presenting with stage I to II MCC, a local recurrence (17 arising within/adjacent to the primary tumor scar) did not appreciably diminish survival compared with patients who had no recurrence (85% vs 88% MCC-specific survival at 5 years).
- Conclusions and relevance: In this cohort study, the MCC recurrence rate (approximately 40%) was notably different than that reported for invasive melanoma (approximately 19%), squamous cell carcinoma (approximately 5%-9%), or basal cell carcinoma (approximately 1%-2%) following definitive therapy. Because more than 90% of MCC recurrences arise within 3 years, it is appropriate to adjust surveillance intensity accordingly. Stage- and time-specific recurrence data can assist in appropriately focusing surveillance resources on patients and time intervals in which recurrence risk is highest.
Scientific and clinical developments in Merkel cell carcinoma: A polyomavirus-driven, often-lethal skin cancer
Akaike T, Nghiem P
J Dermatol Sci. 2022 Jan;105(1):2-10. doi: 10.1016/j.jdermsci.2021.10.004
PMID: 34836718
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a primary neuroendocrine skin cancer that recurs in ~40% of cases. Merkel cell polyomavirus (MCPyV) and ultraviolet (UV)-induced mutations are two major causative factors of MCC. Virus-positive MCCs express polyomavirus oncoproteins that are highly immunogenic yet are required for ongoing tumor growth. Virus-negative MCCs have a high burden of UV-DNA mutations that encode tumor- specific UV-neoantigens. Thus, both UV- and virus-induced MCCs are highly immunogenic, enabling diverse T-cell targeted therapies. Optimal MCC management is challenging given its rarity, aggressive nature, rapidly evolving care guidelines, and fundamental differences in management compared to other skin cancers. MCC is often managed aggressively with extensive surgery, radiotherapy or systemic therapy, frequently leading to toxicities that might have been avoidable while still achieving optimal disease control. Thus, multi-disciplinary care is crucial for providing patients with the best possible outcomes. The outlook for many patients with advanced MCC has progressed remarkably over the past decade due to PD-1 pathway blocking agents that provide durable benefit for a substantial subset of MCC patients. The management of early-stage MCC has also improved due to better approaches to integrate surgery and radiotherapy. Prognostic accuracy and ongoing surveillance have advanced due to stage-specific recurrence data and sophisticated “liquid biopsies” that allow early detection of disease recurrence. Here we summarize both recent striking progress and pressing challenges such as PD-(L)1-refractory MCC, and management of MCC patients with immune dysfunction. We also highlight diverse resources to allow providers to take advantage of recent progress in this fast-moving field.
2021
New interpretable machine-learning method for single-cell data reveals correlates of clinical response to cancer immunotherapy
Greene E, Finak G, D'Amico LA, Bhardwaj N, Church CD, Morishima C, Ramchurren N, Taube JM, Nghiem PT, Cheever MA, Fling SP, Gottardo R
Patterns (N Y). 2021 Oct 27;2(12):100372. doi: 10.1016/j.patter.2021.100372.
PMID: 34950900
Abstract and Highlights
- We introduce a new method for single-cell cytometry studies, FAUST, which performs unbiased cell population discovery and annotation. FAUST processes experimental data on a per-sample basis and returns biologically interpretable cell phenotypes, making it well suited for the analysis of complex datasets. We provide simulation studies that compare FAUST with existing methodology, exemplifying its strength. We apply FAUST to data from a Merkel cell carcinoma anti-PD-1 trial and discover pre-treatment effector memory T cell correlates of outcome co-expressing PD-1, HLA-DR, and CD28. Using FAUST, we then validate these correlates in cryopreserved peripheral blood mononuclear cell samples from the same study, as well as an independent CyTOF dataset from a published metastatic melanoma trial. Finally, we show how FAUST’s phenotypes can be used to perform cross-study data integration in the presence of diverse staining panels. Together, these results establish FAUST as a powerful new approach for unbiased discovery in single-cell cytometry.
Avelumab in patients with previously treated metastatic Merkel cell carcinoma (JAVELIN Merkel 200): updated overall survival data after >5 years of follow-up
S P D'Angelo, S Bhatia, A S Brohl, O Hamid, J M Mehnert, P Terheyden, K C Shih, I Brownell, C Lebbé, K D Lewis, G P Linette, M Milella, H Xiong, G Guezel, P T Nghiem
ESMO Open. 2021 Oct 26;6(6):100290. doi: 10.1016/j.esmoop.2021.100290.
PMID: 34715570
Abstract and Highlights
- Background: Merkel cell carcinoma (MCC) is a rare, aggressive skin cancer that has a poor prognosis in patients with advanced disease. Avelumab [anti-programmed death-ligand 1 (PD-L1)] became the first approved treatment for patients with metastatic MCC (mMCC), based on efficacy and safety data observed in the JAVELIN Merkel 200 trial. We report long-term overall survival (OS) data after >5 years of follow-up from the cohort of patients with mMCC whose disease had progressed after one or more prior lines of chemotherapy.
- Patients and methods: In Part A of the single-arm, open-label, phase II JAVELIN Merkel 200 trial, patients with mMCC that had progressed following one or more prior lines of chemotherapy received avelumab 10 mg/kg by intravenous infusion every 2 weeks until confirmed disease progression, unacceptable toxicity, or withdrawal. In this analysis, long-term OS was analyzed.
- Results: In total, 88 patients were treated with avelumab. At data cut-off (25 September 2020), median follow-up was 65.1 months (range 60.8-74.1 months). One patient (1.1%) remained on treatment, and an additional patient (1.1%) had reinitiated avelumab after previously discontinuing treatment. Median OS was 12.6 months [95% confidence interval (CI) 7.5-17.1 months], with a 5-year OS rate of 26% (95% CI 17% to 36%). In patients with PD-L1+ versus PD-L1- tumors, median OS was 12.9 months (95% CI 8.7-29.6 months) versus 7.3 months (95% CI 3.4-14.0 months), and the 5-year OS rate was 28% (95% CI 17% to 40%) versus 19% (95% CI 5% to 40%), respectively (HR 0.67; 95% CI 0.36-1.25).
- Conclusion: Avelumab monotherapy resulted in meaningful long-term OS in patients with mMCC whose disease had progressed following chemotherapy. These results further support the role of avelumab as a standard of care for patients with mMCC.
Metabolic regulation by PD-1 signaling promotes long-lived quiescent CD8 T cell memory in mice
Kalia V, Yuzefpolskiy Y, Vegaraju A, Xiao H, Baumann F, Jatav S, Church C, Prlic M, Jha A, Nghiem P, Riddell S, Sarkar S
Sci Transl Med. 2021 Oct 13;13(615):eaba6006. doi: 10.1126/scitranslmed.aba6006. Epub 2021 Oct 13.
PMID: 34644150
Abstract and Highlights
- Inhibitory signaling in dysfunctional CD8 T cells through the programmed cell death 1 (PD-1) axis is well established in chronic viral infections and cancers. PD-1 is also transiently induced to high concentrations during priming of acute infections and immunizations, yet its impact on the development of long-lived antigen-independent T cell memory remains unclear. In addition to its expected role in restraining clonal effector expansion, here, we show that PD-1 expression on antigen-specific CD8 T cells is required for the development of a durable CD8 T cell memory pool after antigen clearance. Loss of T cell–specific PD-1 signaling led to increased contraction and a defect in antigen-independent renewal of memory CD8 T cells in response to homeostatic cytokine signals, thus resulting in attrition of the memory pool over time. Whereas exhausted CD8 T cells regain function after PD-1 checkpoint blockade during chronic viral infection, the preexisting pool of resting functional bystander memory CD8 T cells established in response to a previously administered immunogen decreased. Metabolically, PD-1 signals were necessary for regulating the critical balance of mTOR-dependent anabolic glycolysis and fatty acid oxidation programs to meet the bioenergetic needs of quiescent CD8 T cell memory. These results define PD-1 as a key metabolic regulator of protective T cell immunity. Furthermore, these results have potential clinical implications for preexisting CD8 T cell memory during PD-1 checkpoint blockade therapy.
Merkel cell carcinoma can be indolent: A case with 7 locoregional recurrences over 15 years highlights the importance of patient-tailored management
Breneman A, Akaike T, Paulson KG, Breneman DL, Nghiem P
JAAD Case Rep. 2021 Aug 20;16:58-61. doi: 10.1016/j.jdcr.2021.08.009. eCollection 2021 Oct.
PMID: 34522748
Abstract and Highlights
- Patients who experience a recurrence of their Merkel cell carcinoma are often treated aggressively. We report a case of a man with an unusually long course of MCC over 15 years who had his MCC recur around his face or neck 7 times before eventually developing distant spread. Because he had 4 major medical problems at the time his MCC initially appeared, less aggressive therapies were chosen for his recurrences, and there was no evidence of disease for the vast majority of his 15-year course, during which he enjoyed excellent quality of life. This case emphasizes the importance of customizing care in MCC to give patients the best quality and quantity of life possible in their particular situation.
First-line avelumab in a cohort of 116 patients with metastatic Merkel cell carcinoma (JAVELIN Merkel 200): primary and biomarker analyses of a phase II study
D'Angelo SP, Lebbé C, Mortier L, Brohl AS, Fazio N, Grob JJ, Prinzi N, Hanna GJ, Hassel JC, Kiecker F, Georges S, Ellers-Lenz B, Shah P, Güzel G, Nghiem P
J Immunother Cancer. 2021 Jul;9(7):e002646. doi: 10.1136/jitc-2021-002646.
PMID: 34301810
Abstract and Highlights
- Background Avelumab (anti-programmed death ligand 1 (PD-L1)) is approved in multiple countries for the treatment of metastatic Merkel cell carcinoma (mMCC), a rare and aggressive skin cancer. We report efficacy and safety data and exploratory biomarker analyses from a cohort of patients with mMCC treated with first-line avelumab in a phase II trial.
- Methods Patients with treatment-naive mMCC received avelumab 10 mg/kg intravenously every 2 weeks. The primary endpoint was durable response, defined as objective response (complete or partial response; assessed by independent review) lasting ≥6 months. Additional assessments included progression-free survival (PFS), overall survival (OS), safety, and biomarker analyses.
- Results In 116 patients treated with avelumab, median follow-up was 21.2 months (range: 14.9–36.6). Thirty-five patients had a response lasting ≥6 months, giving a durable response rate of 30.2% (95% CI: 22.0% to 39.4%). The objective response rate was 39.7% (95% CI: 30.7% to 49.2%). Median PFS was 4.1 months (95% CI: 1.4 to 6.1) and median OS was 20.3 months (95% CI: 12.4 to not estimable). Response rates were numerically higher in patients with PD-L1+ tumors, Merkel cell polyomavirus (MCPyV)-negative tumors, and tumors with increased intratumoral CD8+ T-cell density. Exploratory analyses did not identify a biomarker that could reliably predict a response to first-line treatment with avelumab; however, a novel gene expression signature to identify the presence of MCPyV+ tumors was derived. Treatment-related adverse events (any grade) occurred in 94 (81.0%) patients, including grade 3/4 events in 21 (18.1%) patients; no treatment-related deaths occurred.
- Conclusion In patients with mMCC, first-line treatment with avelumab led to responses in 40% and durable responses in 30%, and was associated with a low rate of grade 3/4 treatment-related adverse events.
Extended T cell epitope landscape in Merkel cell polyomavirus large T and small T oncoproteins identified uniquely in cancer patients
Hansen UK, Lyngaa R, Ibrani D, Church CD, Verhaegen M, Dlugosz AA, Becker JC, Straten PT, Nghiem P, Hadrup SR
J Invest Dermatol. 2021 Jul 20;S0022-202X(21)01459-7. doi: 10.1016/j.jid.2021.06.027.
PMID: 34298058
Abstract and Highlights
- Merkel Cell carcinoma (MCC) is a rare, aggressive human skin cancer with poor prognosis for advanced disease (Harms et al. 2016). The oncovirus Merkel cell polyomavirus (MCPyV) is associated with at least 80% of MCC cases (Feng et al. 2008) with persistent expression of the viral T antigens (T-Ag; large T antigen (LTA) and small T antigen (STA)) driving oncogenesis (Shuda et al. 2008). Immune surveillance is critical for tumor control. Highlighted by associations between survival and intratumoral levels of CD3+ and CD8+ lymphocytes (Paulson et al. 2014; Sihto and Joensuu 2012), and T-Ag-specific T-cells (Miller et al. 2017). As well as the high efficacy of checkpoint inhibitors (D’Angelo et al. 2018; Nghiem et al. 2016; Topalian et al. 2020). Nevertheless, for half of the patients, this treatment strategy is insufficient. Instead, T-cell-based therapies, such as cell therapies or vaccines, could be attractive, but require identification of CD8+ T-cell epitopes within T-Ag that serve as targets for tumor cell elimination. Several T-Ag-derived epitopes have been identified for a limited number of HLA haplotypes (Iyer et al. 2011; Jing et al. 2020; Lyngaa et al. 2014; Samimi et al. 2019), which reduces such applications to patients with the given HLA haplotypes. In addition, limited evidence is available for natural processing and MHC class I presentation of T-Ag-derived epitopes on MCC tumors, which is essential for T-cell-mediated tumor cell elimination. We, therefore, aimed to expand the repertoire of T-Ag-derived epitopes by creating a library of 146 potential CD8+ T-cell epitopes derived from STA, truncated LTA, including their shared common T antigen (CT) region, and viral capsid protein 1 (VP1) (Figure S1a, and Table S1). The majority of peptides were restricted to the newly evaluated HLA haplotypes, HLA-A*24:02, -B*08:01, -B*35:01, and -B*44:02 (Figure 1a), selected through in-silico predictions of HLA binding. T-cell epitopes restricted to HLA-A*01:01, -A*02:01, -A*03:01, -A*11:01, and -B*07:02 were previously described by Lyngaa et al. Additional HLA-matched control epitopes from common non-oncogenic viruses were included as positive controls for the T-cell detection process.
Intersection of Two Checkpoints: Could Inhibiting the DNA Damage Response Checkpoint Rescue Immune Checkpoint-Refractory Cancer?
Goff PH, Bhakuni R, Pulliam T, Lee JH, Hall ET, Nghiem P
Cancers (Basel). 2021 Jul 8;13(14):3415. doi: 10.3390/cancers13143415.
PMID: 34298632
Abstract and Highlights
- Metastatic cancers resistant to immunotherapy require novel management strategies. DNA damage response (DDR) proteins, including ATR (ataxia telangiectasia and Rad3-related), ATM (ataxia telangiectasia mutated) and DNA-PK (DNA-dependent protein kinase), have been promising therapeutic targets for decades. Specific, potent DDR inhibitors (DDRi) recently entered clinical trials. Surprisingly, preclinical studies have now indicated that DDRi may stimulate anti-tumor immunity to augment immunotherapy. The mechanisms governing how DDRi could promote anti-tumor immunity are not well understood; however, early evidence suggests that they can potentiate immunogenic cell death to recruit and activate antigen-presenting cells to prime an adaptive immune response. Merkel cell carcinoma (MCC) is well suited to test these concepts. It is inherently immunogenic as ~50% of patients with advanced MCC persistently benefit from immunotherapy, making MCC one of the most responsive solid tumors. As is typical of neuroendocrine cancers, dysfunction of p53 and Rb with upregulation of Myc leads to the very rapid growth of MCC. This suggests high replication stress and susceptibility to DDRi and DNA-damaging agents. Indeed, MCC tumors are particularly radiosensitive. Given its inherent immunogenicity, cell cycle checkpoint deficiencies and sensitivity to DNA damage, MCC may be ideal for testing whether targeting the intersection of the DDR checkpoint and the immune checkpoint could help patients with immunotherapy-refractory cancers.
Spatial transcriptomics at subspot resolution with BayesSpace
Zhao E, Stone MR, Ren X, Guenthoer J, Smythe KS, Pulliam T, Williams SR, Uytingco CR, Taylor S, Nghiem P, Bielas JH, Gottardo R
Nat Biotechnol. 2021 Jun 3. doi: 10.1038/s41587-021-00935-2.
PMID: 34083791
Abstract and Highlights
- Recent spatial gene expression technologies enable comprehensive measurement of transcriptomic profiles while retaining spatial context. However, existing analysis methods do not address the limited resolution of the technology or use the spatial information efficiently. Here, we introduce BayesSpace, a fully Bayesian statistical method that uses the information from spatial neighborhoods for resolution enhancement of spatial transcriptomic data and for clustering analysis. We benchmark BayesSpace against current methods for spatial and non-spatial clustering and show that it improves identification of distinct intra-tissue transcriptional profiles from samples of the brain, melanoma, invasive ductal carcinoma and ovarian adenocarcinoma. Using immunohistochemistry and an in silico dataset constructed from scRNA-seq data, we show that BayesSpace resolves tissue structure that is not detectable at the original resolution and identifies transcriptional heterogeneity inaccessible to histological analysis. Our results illustrate BayesSpace’s utility in facilitating the discovery of biological insights from spatial transcriptomic datasets.
Three-year survival, correlates and salvage therapies in patients receiving first-line pembrolizumab for advanced Merkel cell carcinoma
Nghiem P, Bhatia S, Lipson EJ, Sharfman WH, Kudchadkar RR, Brohl AS, Friedlander PA, Daud A, Kluger HM, Reddy SA, Boulmay BC, Riker A, Burgess MA, Hanks BA, Olencki T, Kendra K, Church C, Akaike T, Ramchurren N, Shinohara MM, Salim B, Taube JM, Jensen E, Kalabis M, Fling SP, Moreno BH, Sharon E, Cheever MA, Topalian SL
J Immunother Cancer. 2021; 9(4): e002478.
PMID: 33879601
Abstract and Highlights
- Background: Merkel cell carcinoma (MCC) is an aggressive skin cancer associated with poor survival. Programmed cell death-1 (PD-1) pathway inhibitors have shown high rates of durable tumor regression compared with chemotherapy for MCC. The current study was undertaken to assess baseline and on-treatment factors associated with MCC regression and 3-year survival, and to explore the effects of salvage therapies in patients experiencing initial non-response or tumor progression after response or stable disease following first-line pembrolizumab therapy on Cancer Immunotherapy Trials Network-09/KEYNOTE-017.
- Methods: In this multicenter phase II trial, 50 patients with advanced unresectable MCC received pembrolizumab 2 mg/kg every 3 weeks for ≤2 years. Patients were followed for a median of 31.8 months.
- Results: Overall response rate to pembrolizumab was 58% (complete response 30%+partial response 28%; 95% CI 43.2 to 71.8). Among 29 responders, the median response duration was not reached (NR) at 3 years (range 1.0+ to 51.8+ months). Median progression-free survival (PFS) was 16.8 months (95% CI 4.6 to 43.4) and the 3-year PFS was 39.1%. Median OS was NR; the 3-year OS was 59.4% for all patients and 89.5% for responders. Baseline Eastern Cooperative Oncology Group performance status of 0, greater per cent tumor reduction, completion of 2 years of treatment and low neutrophil-to-lymphocyte ratio were associated with response and longer survival. Among patients with initial disease progression or those who developed progression after response or stable disease, some had extended survival with subsequent treatments including chemotherapies and immunotherapies.
- Conclusions: This study represents the longest available follow-up from any first-line anti-programmed death-(ligand) 1 (anti-PD-(L)1) therapy in MCC, confirming durable PFS and OS in a proportion of patients. After initial tumor progression or relapse following response, some patients receiving salvage therapies survived. Improving the management of anti-PD-(L)1-refractory MCC remains a challenge and a high priority.
Quality Is King: Fundamental Insights into Tumor Antigenicity from Virus-Associated Merkel Cell Carcinoma
Lahman MC, Paulson KG, Nghiem PT, Chapuis AG
J Invest Dermatol. 2021 Apr 13;S0022-202X(21)00999-4. doi: 10.1016/j.jid.2020.12.037
PMID: 33863500
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a rare skin malignancy that is a paradigm cancer for solid tumor immunotherapy. MCCs associated with Merkel cell polyomavirus (virus-positive MCC [VP-MCC]) or chronic UV exposure (virus-negative MCC [VN-MCC]) are anti-PD(L)1 responsive, despite VP-MCC’s low mutational burden. This suggests that antigen quality, not merely mutation quantity, dictates immunotherapy responsiveness, and cell-based therapies targeting optimal antigens may be effective. Despite VP-MCC’s antigenic homogeneity, diverse T-cell infiltration patterns are observed, implying microenvironment plasticity and multifactorial contributions to immune recognition. Moreover, VP-MCC exemplifies how antitumor adaptive immunity can provide tumor burden biomarkers for early detection and disease monitoring.
How we treat Merkel cell carcinoma: within and beyond current guidelines
Park SY, Doolittle-Amieva C, Moshiri Y, Akaike T, Parvathaneni U, Bhatia S, Zaba L, Nghiem P
Future Oncol. doi: 10.2217/fon-2020-1036
PMID: 33511866
Abstract and Highlights
- Merkel cell carcinoma (MCC) is an aggressive skin cancer associated with a high risk of local recurrence and distant metastasis. Optimal care of this potentially life-threatening cancer is critical but challenging because: physicians are often unfamiliar with its management due to rarity, and MCC management remains controversial, in part because it is rapidly evolving across multiple specialties. While guidelines offer a broad overview of management, they are often not sufficient when making decisions for individual patients. Herein, we present a literature review as well as practical approaches adopted at our institutions for staging, surveillance and therapy of MCC. Each of these areas are discussed in light of how they can be appropriately customized for prevalent but challenging situations. We also provide representative examples of MCC patient scenarios and how they were managed by a multidisciplinary team to identify suitable evidence-based, individualized treatment plans.
Folate hydrolase-1 (FOLH1) is a novel target for antibody-based brachytherapy in Merkel cell carcinoma
M K Ramirez-Fort, B Meier-Schiesser, K Lachance, S S Mahase, C D Church, M J Niaz, H Liu, V Navarro, A Nikolopoulou , D V Kazakov, E Contassot, D P Nguyen, J Sach, L Hadravsky, Y Sheng, S T Tagawa, X Wu, C S Lange, L E French, P T Nghiem, N H Bander
Skin Health Dis. 2021 Mar;1(1):e9. doi: 10.1002/ski2.9. Epub 2020 Nov 28.
PMID: 34541577
Abstract and Highlights
- Backgrounds: Folate Hydrolase-1 (FOLH1; PSMA) is a type II transmembrane protein, luminally expressed by solid tumour neo-vasculature. Monoclonal antibody (mAb), J591, is a vehicle for mAb-based brachytherapy in FOLH1+ cancers. Brachytherapy is a form of radiotherapy that involves placing a radioactive material a short distance from the target tissue (e.g., on the skin or internally); brachytherapy is commonly accomplished with the use of catheters, needles, metal seeds and antibody or small peptide conjugates. Herein, FOLH1 expression in primary (p) and metastatic (m) Merkel cell carcinoma (MCC) is characterized to determine its targeting potential for J591-brachytherapy.
- Materials & methods: Paraffin sections from pMCC and mMCC were evaluated by immunohistochemistry for FOLH1. Monte Carlo simulation was performed using the physical properties of conjugated radioisotope lutetium-177. Kaplan-Meier survival curves were calculated based on patient outcome data and FOLH1 expression.
- Results: Eighty-one MCC tumours were evaluated. 67% (54/81) of all cases, 77% (24/31) pMCC and 60% (30/50) mMCC tumours were FOLH1+. Monte Carlo simulation showed highly localized ionizing tracks of electrons emitted from the targeted neo-vessel. 42% (34/81) of patients with FOLH1+/- MCC had available survival data f or analysis. No significant differences in our limited data set were detected based on FOLH1 status (p = 0.4718; p = 0.6470), staining intensity score (p = 0.6966; p = 0.9841) or by grouping staining intensity scores (- and + vs. ++, +++, +++) (p = 0.8022; p = 0.8496) for MCC-specific survival or recurrence free survival, respectively.
- Conclusions: We report the first evidence of prevalent FOLH1 expression within MCC-associated neo-vessels, in 60-77% of patients in a large MCC cohort. Given this data, and the need for alternatives to immune therapies it is appropriate to explore the safety and efficacy o f FOLH1-targeted brachytherapy for MCC.
Immune checkpoint inhibitor therapy in HIV-associated Merkel cell carcinoma: A case series of 3 patients
Song Y Park, Candice Church, Nora A Alexander, Michi M Shinohara, Kelly G Paulson, Karl D Lewis, Nancy S Lee, Paul Nghiem
JAAD Case Rep. 2021 Feb; 8: 28–33.
PMID: 33490342
Abstract and Highlights
- Merkel cell carcinoma (MCC) is an aggressive skin cancer, which is about twice as likely to metastasize as compared with melanoma.1 There are 2 distinct biological pathways for developing MCC: Merkel cell polyomavirus (MCPyV)-induced and ultraviolet light-induced.2 In individuals immunosuppressed by HIV infection, the risk of developing MCC is 13-fold higher than for the general population.1 Historically, outcomes have been dismal, with a 2-year disease-specific survival rate of 0% in 1 published case series.3
- Recently, anti-programmed cell death 1 (PD-1) and anti-programmed death ligand 1 (PD-L1) agents in immunocompetent patients with advanced MCC (aMCC) demonstrated a ∼60% response rate and a durable benefit in the majority of responding patients.4 Based on these data, these agents have emerged as the treatment of choice for aMCC. However, immunosuppressed individuals, including those who are HIV-positive, have been excluded from clinical trials with anti-PD-(L)1 agents due to concerns about efficacy and potential for inadvertent augmentation of infectious and/or inflammatory activity.5 It is, therefore, unknown whether immune checkpoint inhibitors (ICI), including anti-PD-(L)1 treatment, are effective for HIV-positive patients with aMCC.
- To better understand the clinical and biological features of HIV-positive aMCC patients treated with ICI, we performed a comprehensive review of our Seattle-based IRB-approved repository of MCC patient data and specimens. We have also described biomarker analyses, including immune cell infiltration, tumor MCPyV status, and intratumoral expression of PD-1 and PD-L1.
Narrow excision margins are appropriate for Merkel cell carcinoma when combined with adjuvant radiation: Analysis of 188 cases of localized disease and proposed management algorithm
Erica S Tarabadkar, Teresa Fu, Kristina Lachance, Daniel S Hippe, Thomas Pulliam, Hannah Thomas, Janet Y Li, Christopher W Lewis, Coley Doolittle-Amieva, David R Byrd, Jeremy T Kampp, Upendra Parvathaneni, Paul Nghiem
J Am Acad Dermatol. 2021 Feb;84(2):340-347. doi: 10.1016/j.jaad.2020.07.079.
PMID: 32711093
Abstract and Highlights
- Background: Merkel cell carcinoma (MCC) management typically includes surgery with or without adjuvant radiation therapy (aRT). Major challenges include determining surgical margin size and whether aRT is indicated.
- Objective: To assess the association of aRT, surgical margin size, and MCC local recurrence.
- Methods: Analysis of 188 MCC cases presenting without clinical nodal involvement.
- Results: aRT-treated patients tended to have higher-risk tumors (larger diameter, positive microscopic margins, immunosuppression) yet had fewer local recurrences (LRs) than patients treated with surgery only (1% vs 15%; P = .001). For patients who underwent surgery alone, 7 of 35 (20%) treated with narrow margins (defined as ≤1.0 cm) developed LR, whereas 0 of 13 patients treated with surgical margins greater than 1.0 cm developed LR (P = .049). For aRT-treated patients, local control was excellent regardless of surgical margin size; only 1% experienced recurrence in each group (1 of 70 with narrow margins ≤1 cm and 1 of 70 with margins >1 cm; P = .56).
- Limitations: This was a retrospective study.
- Conclusions: Among patients treated with aRT, local control was superb even if significant risk factors were present and margins were narrow. We propose an algorithm for managing primary MCC that integrates risk factors and optimizes local control while minimizing morbidity.
Lack of efficacy of radiation therapy plus PD-L1 blockade for Merkel cell carcinoma arising in a patient with chronic active Epstein-Barr virus infection
Okazaki A, Nakai K, Kusutani N, Kamo R, Fukunaga Y, Nagase K, Nghiem P, Tsuruta D.
Dermatol Ther. 2020 Dec 29;e14722.doi: 10.1111/dth.14722
PMID: 33373098
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a rare and aggressive skin cancer that occurs in elderly patients. The risk of MCC is increased by immunosuppression due to conditions such as human immunodeficiency virus infection, hematological malignancies, and organ transplantation. These risk factors can also be associated with a poor prognosis in MCC. Chronic active Epstein-Barr virus (CAEBV) infection is a rare Epstein-Barr virus (EBV) infectious disease characterized by persistent infectious mononucleosis-like symptoms. Recently, programmed cell death ligand 1 (PD-L1) blockade using avelumab was approved as the first-line therapy for patients with metastatic MCC. Here, we report a case of extremely hyperprogressive MCC occurring in a patient with CAEBV.
2020
PD-1 and TIGIT coexpression identifies a circulating CD8 T cell subset predictive of response to anti-PD-1 therapy
Simon S, Voillet V, Vignard V, Wu Z, Dabrowski C, Jouand N, Beauvais T, Khammari A, Braudeau C, Josien R, Adotevi O, Laheurte C, Aubin F, Nardin C, Rulli S, Gottardo R, Ramchurren N, Cheever M, Fling SP, Church CD, Nghiem P, Dreno B, Riddell SR, Labarriere N
J Immunother Cancer. 2020 Nov;8(2):e001631. doi: 10.1136/jitc-2020-001631.
PMID: 33188038
Health-related quality of life trajectory of treatment-naive patients with Merkel cell carcinoma receiving avelumab
Murtuza Bharmal, Sandra Nolte, Céleste Lebbé, Laurent Mortier, Andrew S Brohl, Nicola Fazio, Jean-Jacquez Grob, Sara Pusceddu, Glenn J Hanna, Jessica C Hassel, Felix Kiecker, Barbara Ellers-Lenz, Marcis Bajars, Gülseren Güzel, Paul Nghiem, Matthias Hunger, Michael Schlichting, Mickaël Henry-Szatkowski, Sandra P D'Angelo
Future Oncol. 2020 Sep;16(27):2089-2099. doi: 10.2217/fon-2020-0426. Epub 2020 Sep 17.
PMID: 32938212
Abstract and Highlights
- Aim: To evaluate changes in health-related quality of life (HRQoL) in a Phase II trial (NCT02155647) of treatment-naive patients with metastatic Merkel cell carcinoma treated with avelumab (15-month follow-up).
- Materials & methods: Mixed-effect Models for Repeated Measures were applied to HRQoL data (FACT-M; EQ-5D-5L) to assess changes over time. Clinically derived progression-free survival was compared with HRQoL deterioration-free survival.
- Results: Overall, we saw relative stability in HRQoL among 116 included patients, with nonprogression associated with statistically and clinically meaningful better HRQoL compared with progressive disease. Deterioration-free survival rates (49-72% at 6 months, 40-58% at 12 months) were consistently higher/better compared with progression-free survival rates (41/31% at 6/12 months).
- Conclusion: These findings show unique longitudinal HRQoL data for treatment-naive metastatic Merkel cell carcinoma patients treated with avelumab. Clinical trial registration: NCT02155647 (ClinicalTrials.gov).
Postoperative, Single-Fraction Radiation Therapy in Merkel Cell Carcinoma of the Head and Neck
Cook MM, Schaub SK, Goff PH, Fu A, Park SY, Hippe DS, Liao JJ, Apisarnthanarax S, Bhatia S, Tseng YD, Nghiem PT, Parvathaneni U
Adv Radiat Oncol. 2020 Jul 21 doi: 10.1016/j.adro.2020.07.003
PMID: 32838069
Abstracts and Highlights
- Purpose: Conventionally fractionated, postoperative radiation therapy (cPORT; 50 Gy in 25 fractions) is considered for patients with Merkel cell carcinoma (MCC) to improve locoregional control. However, cPORT is associated with acute toxicity, especially in the head and neck (H&N) region, and requires daily treatments over several weeks. We previously reported high rates of durable local control with minimal toxicity using 8-Gy single-fraction radiation therapy (SFRT) in the metastatic setting. We report early results on a cohort of patients with localized H&N MCC who received postoperative SFRT if a cPORT regimen was not feasible.
- Methods and materials: Twelve patients with localized MCC of the H&N (clinical/pathologic stages I-II) and no prior radiation therapy to the region were identified from an institutional review board-approved prospective registry who underwent surgical resection followed by postoperative SFRT. Time to event was calculated starting from the date of resection before SFRT. The cumulative incidence of in-field locoregional recurrences and out-of-field recurrences was estimated with death as a competing risk.
- Results: Twelve patients with H&N MCC were identified with clinical/pathologic stages I-II H&N MCC. Median age at diagnosis was 81 years (range, 58-96 years); 25% had immunosuppression. At a median follow-up of 19 months (range, 8-34), there were no in-field locoregional recurrences. A single out-of-field regional recurrence was observed, which was successfully salvaged. There were no MCC-specific deaths. No radiation-associated toxicities greater than grade 1 (Common Terminology Criteria for Adverse Events v5) were observed.
- Conclusions: Preliminary data suggest that SFRT could offer a potential alternative to cPORT to treat the primary site for localized H&N MCC, particularly in elderly or frail patients, with promising in-field local control and minimal toxicity. Further data with validation in larger cohorts are needed to confirm the sustained safety and efficacy of postoperative SFRT.
Clinical Benefit of Baseline Imaging in Merkel Cell Carcinoma: Analysis of 584 Patients
Neha Singh, BS, Nora A. Alexander, BS, Kristina Lachance, MS, Christopher W. Lewis, MD, Aubriana McEvoy, MD, Gensuke Akaike, MD, David Byrd, MD, Sanaz Behnia, MD, Shailender Bhatia, MD, Kelly G. Paulson, MD, PhD, Paul Nghiem, MD, PhD
J Am Acad Dermatol . 2020 Jul 21;S0190-9622(20)32265-9. doi: 10.1016/j.jaad.2020.07.065.
PMID: 32707254
Abstract and Highlights
- BACKGROUND: Merkel cell carcinoma (MCC) guidelines derive from melanoma and do not recommend baseline cross-sectional imaging for most patients. However, MCC is more likely to have metastasized at diagnosis than melanoma.
- OBJECTIVE: To determine how often baseline imaging identifies clinically occult MCC in newly diagnosed patients with and without palpable nodal involvement.
- METHODS: Analysis of 584 MCC patients with a cutaneous primary, baseline imaging, no evident distant metastases, and sufficient staging data.
- RESULTS: Among 492 patients with clinically uninvolved regional nodes, 13.2% were upstaged by imaging (8.9% in regional nodes, 4.3% in distant sites). Among 92 patients with clinically involved regional nodes, 10.8% were upstaged to distant metastatic disease. Large (>4cm) and small (<1cm) primary tumors were both frequently upstaged (29.4% and 7.8%, respectively). PET-CT upstaged patients more often (16.8% of 352), than CT alone (6.9% of 231; p=0.0006).
- LIMITATIONS: This was a retrospective study.
- CONCLUSIONS: In clinically node-negative patients, baseline imaging revealed occult metastatic MCC at a higher rate than reported for melanoma (13.2% vs. <1%). Although imaging is already recommended for clinically node-positive MCC patients, these data suggest that baseline imaging is also indicated for clinically node-negative patients because upstaging is frequent and markedly alters management and prognosis.
The 6-4 Photoproduct Is the Trigger of UV-induced Replication Blockage and ATR Activation
Kai-Feng Hunga, Julia M. Sidorova, Paul Nghiem, and Masaoki Kawasumi
Proc Natl Acad Sci. 2020 May 22;201917196. doi: 10.1073/pnas.1917196117.
PMID: 32444488
Abstract and Highlights
- The most prevalent human carcinogen is sunlight-associated ultraviolet (UV), a physiologic dose of which generates thousands of DNA lesions per cell, mostly of two types: cyclobutane pyrimidine dimers (CPDs) and 6-4 photoproducts (6-4PPs). It has not been possible, in living cells, to precisely characterize the respective contributions of these two lesion types to the signals that regulate cell cycle progression, DNA replication, and cell survival. Here we coupled multiparameter flow cytometry with lesion-specific photolyases that eliminate either CPDs or 6-4PPs and determined their respective contributions to DNA damage responses. Strikingly, only 6-4PP lesions activated the ATR-Chk1 DNA damage response pathway. Mechanistically, 6-4PPs, but not CPDs, impeded DNA replication across the genome as revealed by microfluidic-assisted replication track analysis. Furthermore, single-stranded DNA accumulated preferentially at 6-4PPs during DNA replication, indicating selective and prolonged replication blockage at 6-4PPs. These findings suggest that 6-4PPs, although eightfold fewer in number than CPDs, are the trigger for UV-induced DNA damage responses.
Avelumab in patients with previously treated metastatic Merkel cell carcinoma: long-term data and biomarker analyses from the single-arm phase 2 JAVELIN Merkel 200 trial.
D'Angelo SP, Bhatia S, Brohl AS, Hamid O, Mehnert JM, Terheyden P, Shih KC, Brownell I, Lebbé C, Lewis KD, Linette GP, Milella M, Georges S, Shah P, Ellers-Lenz B, Bajars M, Güzel G, Nghiem PT
J Immunother Cancer . 2020 May;8(1):e000674. doi: 10.1136/jitc-2020-000674.
PMID: 32414862
Abstract and Highlights
- Background: Merkel cell carcinoma (MCC) is a rare, aggressive skin cancer associated with a high risk of metastasis. In 2017, avelumab (anti-programmed death-ligand 1 (PD-L1)) became the first approved treatment for patients with metastatic MCC (mMCC), based on the occurrence of durable responses in a subset of patients. Here, we report long-term efficacy and safety data and exploratory biomarker analyses in patients with mMCC treated with avelumab.
- Methods: In a cohort of this single-arm, phase 2 trial (JAVELIN Merkel 200), patients with mMCC and disease progression after prior chemotherapy received avelumab 10 mg/kg intravenously every 2 weeks. The primary endpoint was confirmed objective response rate (ORR) by independent review per Response Evaluation Criteria in Solid Tumors V.1.1. Other assessments included duration of response, progression-free survival, overall survival (OS), safety and biomarker analyses.
- Results: As of 14 September 2018, 88 patients had been followed up for a median of 40.8 months (range 36.4-49.7 months). The ORR was 33.0% (95% CI 23.3% to 43.8%), including a complete response in 11.4% (10 patients), and the median duration of response was 40.5 months (95% CI 18.0 months to not estimable). As of 2 May 2019 (≥44 months of follow-up), the median OS was 12.6 months (95% CI 7.5 to 17.1 months) and the 42-month OS rate was 31% (95% CI 22% to 41%). Of long-term survivors (OS >36 months) evaluable for PD-L1 expression status (n=22), 81.8% had PD-L1+ tumors. In exploratory biomarker analyses, high tumor mutational burden (≥2 non-synonymous somatic variants per megabase) and high major histocompatibility complex class I expression (30% of tumors with highest expression) were associated with trends for improved ORR and OS. In long-term safety assessments (≥36 months of follow-up), no new or unexpected adverse events were reported, and no treatment-related deaths occurred.
- Conclusions: Avelumab showed continued durable responses and meaningful long-term survival outcomes in patients with mMCC, reinforcing avelumab as a standard-of-care treatment option for this disease.
Neoadjuvant Nivolumab for Patients With Resectable Merkel Cell Carcinoma in the CheckMate 358 Trial
Topalian SL, Bhatia S, Amin A, Kudchadkar RR, Sharfman WH, Lebbé C, Delord JP, Dunn LA, Shinohara MM, Kulikauskas R, Chung CH, Martens UM, Ferris RL, Stein JE, Engle EL, Devriese LA, Lao CD, Gu J, Li B, Chen T, Barrows A, Horvath A, Taube JM, Nghiem
J Clin Oncol. 2020 Apr 23:JCO2000201. doi: 10.1200/JCO.20.00201
PMID: 32324435
Abstract and Highlights
- PURPOSE: Merkel cell carcinoma (MCC) is a rare, aggressive skin cancer commonly driven by the Merkel cell polyomavirus (MCPyV). The programmed death-1 (PD-1)/programmed death-ligand 1 (PD-L1) immunosuppressive pathway is often upregulated in MCC, and advanced metastatic MCC frequently responds to PD-1 blockade. We report what we believe to be the first trial of anti-PD-1 in the neoadjuvant setting for resectable MCC.
- METHODS: In the phase I/II CheckMate 358 study of virus-associated cancer types, patients with resectable MCC received nivolumab 240 mg intravenously on days 1 and 15. Surgery was planned on day 29. Tumor regression was assessed radiographically and microscopically. Tumor MCPyV status, PD-L1 expression, and tumor mutational burden (TMB) were assessed in pretreatment tumor biopsies.
- RESULTS: Thirty-nine patients with American Joint Committee on Cancer stage IIA-IV resectable MCC received ≥ 1 nivolumab dose. Three patients (7.7%) did not undergo surgery because of tumor progression (n = 1) or adverse events (n = 2). Any-grade treatment-related adverse events occurred in 18 patients (46.2%), and grade 3-4 events in 3 patients (7.7%), with no unexpected toxicities. Among 36 patients who underwent surgery, 17 (47.2%) achieved a pathologic complete response (pCR). Among 33 radiographically evaluable patients who underwent surgery, 18 (54.5%) had tumor reductions ≥ 30%. Responses were observed regardless of tumor MCPyV, PD-L1, or TMB status. At a median follow-up of 20.3 months, median recurrence-free survival (RFS) and overall survival were not reached. RFS significantly correlated with pCR and radiographic response at the time of surgery. No patient with a pCR had tumor relapse during observation.
- CONCLUSION: Nivolumab administered approximately 4 weeks before surgery in MCC was generally tolerable and induced pCRs and radiographic tumor regressions in approximately one half of treated patients. These early markers of response significantly predicted improved RFS. Additional investigation of these promising findings is warranted.
- Supplementary Material can be found here
- Additional commentary can be found here
High somatostatin receptor expression and efficacy of somatostatin analogues in patients with metastatic Merkel cell carcinoma
T Akaike, J Qazi, A Anderson, F S Behnia, M M Shinohara, G Akaike, D S Hippe, H Thomas, S R Takagishi, K Lachance, S Y Park, E S Tarabadkar, J G Iyer, A Blom, U Parvathaneni, H Vesselle, P Nghiem, S Bhatia
Br J Dermatol. 2020 Apr 22. doi: 10.1111/bjd.19150.
PMID: 32320473
Abstract and Highlights
- Background: Merkel cell carcinoma (MCC) is an aggressive, high-grade, cutaneous neuroendocrine tumour (NET). Agents blocking programmed death 1/programmed death ligand 1 have efficacy in metastatic MCC (mMCC), but half of patients do not derive durable benefit. Somatostatin analogues (SSAs) are commonly used to treat low- and moderate-grade NETs that express somatostatin receptors (SSTRs).
- Objectives: To assess SSTR expression and the efficacy of SSAs in mMCC, a high-grade NET. Methods In this retrospective study of 40 patients with mMCC, SSTR expression was assessed radiologically by somatostatin receptor scintigraphy (SRS; n = 39) and/or immunohistochemically when feasible (n = 9). Nineteen patients (18 had SRS uptake in MCC tumours) were treated with SSA. Disease control was defined as progression-free survival (PFS) of ≥ 120 days after initiation of SSA.
- Results: Thirty-three of 39 patients (85%) had some degree (low 52%, moderate 23%, high 10%) of SRS uptake. Of 19 patients treated with SSA, seven had a response-evaluable target lesion; three of these seven patients (43%) experienced disease control, with a median PFS of 237 days (range 152-358). Twelve of 19 patients did not have a response-evaluable lesion due to antecedent radiation; five of these 12 (42%) experienced disease control (median PFS of 429 days, range 143-1757). The degree of SSTR expression (determined by SRS and/or immunohistochemistry) did not correlate significantly with the efficacy endpoints.
- Conclusions: In contrast to other high-grade NETs, mMCC tumours appear frequently to express SSTRs. SSAs can lead to clinically meaningful disease control with minimal side-effects. Targeting of SSTRs using SSA or other novel approaches should be explored further for mMCC.
Polyomavirus‐driven Merkel cell carcinoma: Prospects for therapeutic vaccine development
Tabachnick‐Cherny S, Pulliam T, Church C, Koelle D, Nghiem P
Mol Carcinog. 2020 Mar 27. doi: 10.1002/mc.23190.
PMID: 32219902
Abstract and Highlights
- Great strides have been made in cancer immunotherapy including the breakthrough successes of anti‐PD‐(L)1 checkpoint inhibitors. In Merkel cell carcinoma (MCC), a rare and aggressive skin cancer, PD‐(L)1 blockade is highly effective. Yet, ~50% of patients either do not respond to therapy or develop PD‐(L)1 refractory disease and, thus, do not experience long‐term benefit. For these patients, additional or combination therapies are needed to augment immune responses that target and eliminate cancer cells. Therapeutic vaccines targeting tumor‐associated antigens, mutated self‐antigens, or immunogenic viral oncoproteins are currently being developed to augment T‐cell responses. Approximately 80% of MCC cases in the United States are driven by the ongoing expression of viral T‐antigen (T‐Ag) oncoproteins from genomically integrated Merkel cell polyomavirus (MCPyV). Since T‐Ag elicits specific B‐ and T‐cell immune responses in most persons with virus‐positive MCC (VP‐MCC), and ongoing T‐Ag expression is required to drive VP‐MCC cell proliferation, therapeutic vaccination with T‐Ag is a rational potential component of immunotherapy. Failure of the endogenous T‐cell response to clear VP‐MCC (allowing clinically evident tumors to arise) implies that therapeutic vaccination will need to be potent anśd synergize with other mechanisms to enhance T‐cell activity against tumor cells. Here, we review the relevant underlying biology of VP‐MCC, potentially applicable therapeutic vaccine platforms, and antigen delivery formats. We also describe early successes in the field of therapeutic cancer vaccines and address several clinical scenarios in which VP‐MCC patients could potentially benefit from a therapeutic vaccine.
Intratumoral Delivery of Plasmid IL12 Via Electroporation Leads to Regression of Injected and Noninjected Tumors in Merkel Cell Carcinoma
Shailender B, Longino NV, Miller NJ, Kulikauskas R, Iyer JG, Ibrani D, Blom A, Byrd DR, Parvathaneni U, Twitty CG, Campbell JS, Le MH, Gargosky S, Pierce RH, Heller R, Daud AI, and Nghiem P
Clin Cancer Res. 2020 Feb 1;26(3):598-607. doi: 10.1158/1078-0432.CCR-19-0972.
PMID: 31582519
Abstract and Highlights
- Purpose: IL12 promotes adaptive type I immunity and has demonstrated antitumor efficacy, but systemic administration leads to severe adverse events (AE), including death. This pilot trial investigated safety, efficacy, and immunologic activity of intratumoral delivery of IL12 plasmid DNA (tavo) via in vivo electroporation (i.t.-tavo-EP) in patients with Merkel cell carcinoma (MCC), an aggressive virus-associated skin cancer.
- Patients and methods: Fifteen patients with MCC with superficial injectable tumor(s) received i.t.-tavo-EP on days 1, 5, and 8 of each cycle. Patients with locoregional MCC (cohort A, N = 3) received one cycle before definitive surgery in week 4. Patients with metastatic MCC (cohort B, N = 12) received up to four cycles total, administered at least 6 weeks apart. Serial tumor and blood samples were collected.
- Results: All patients successfully completed at least one cycle with transient, mild (grades 1 and 2) AEs and without significant systemic toxicity. Sustained (day 22) intratumoral expression of IL12 protein was observed along with local inflammation and increased tumor-specific CD8+ T-cell infiltration, which led to systemic immunologic and clinical responses. The overall response rate was 25% (3/12) in cohort B, with 2 patients experiencing durable clinical benefit (16 and 55+ months, respectively). Two cohort A patients (1 with pathologic complete remission) were recurrence-free at 44+ and 75+ months, respectively.
- Conclusions: I.t.-tavo-EP was safe and feasible without systemic toxicity. Sustained local expression of IL12 protein and local inflammation led to systemic immune responses and clinically meaningful benefit in some patients. Gene electrotransfer, specifically i.t.-tavo-EP, warrants further investigation for immunotherapy of cancer.
2019
Patterns of distant metastases in 215 Merkel cell carcinoma patients: Implications for prognosis and surveillance
Lewis CW, Qazi J, Hippe DS, Lachance K, Thomas H, Cook MM, Juhlin I, Singh N, Thuesmunn Z, Takagishi SR, McEvoy A, Doolittle-Amieva C, Bhatia S, Paulson KG, O'Malley RB, Wang CL, Nghiem P
Cancer Med. 2019 Dec 27. doi: 10.1002/cam4.2781.
PMID: 31883234
Abstract and Highlights
- Approximately one-third of Merkel cell carcinoma (MCC) patients eventually develop distant metastatic disease. Little is known about whether the location of the primary lesion is predictive of initial distant metastatic site, or if survival likelihood differs depending on the metastatic site. Such data could inform imaging/surveillance practices and improve prognostic accuracy. Multivariate and competing-risk analyses were performed on a cohort of 215 MCC patients with distant metastases, 31% of whom had two or more initial sites of distant metastasis. At time of initial distant metastasis in the 215 patients, metastatic sites (n = 305) included non-regional lymph nodes (present in 41% of patients), skin/body wall (25%), liver (23%), bone (21%), pancreas (8%), lung (7%), and brain (5%). Among the 194 patients who presented with MCC limited to local or regional sites (stage I-III) but who ultimately developed distant metastases, distant progression occurred in 49% by 1 year and in 80% by 2 years following initial diagnosis. Primary MCC locations differed in how likely they were to metastasize to specific organs/sites (P < .001). For example, liver metastases were far more likely from a head/neck primary (43% of 58 patients) versus a lower limb primary (5% of 39 patients; P < .0001). Skin-only distant metastasis was associated with lower MCC-specific mortality as compared to metastases in multiple organs/sites (HR 2.7; P = .003), in the liver (HR 2.1; P = .05), or in distant lymph nodes (HR 2.0; P = .045). These data reflect outcomes before PD1-pathway inhibitor availability, which may positively impact survival. In conclusion, primary MCC location is associated with a pattern of distant spread, which may assist in optimizing surveillance. Because it is linked to survival, the site of initial distant metastasis should be considered when assessing prognosis.
Identification of Therapeutic Vulnerabilities in Small Cell Neuroendocrine Prostate Cancer
Corella AN, Cabiliza Ordonio MVA, Coleman I, Lucas JM, Kaipainen A, Nguyen HM, Sondheim D, Brown L, True LD, Lee JK, MacPherson D, Nghiem P, Gulati R, Morrissey C, Corey E, Nelson PS
Clin Cancer Res. 2019 Dec 5. pii: clincanres.0775.2019. doi: 10.1158/1078-0432.CCR-19-0775
PMID: 31806643
Abstract and Highlights
- Purpose: Small-cell neuroendocrine prostate cancer (SCNPC) exhibits an aggressive clinical course and incidence rates appear to be increasing following resistance to potent androgen receptor (AR) antagonists. Currently, treatment options are limited and few model systems are available to identify new approaches for treatment. We sought to evaluate commonalities between SCNPC and other aggressive neuroendocrine carcinomas to identify therapeutic targets.
- Experimental Design: We generated whole transcriptome RNAseq data from AR-active prostate cancers (ARPC) and SCNPCs from tumors collected at rapid autopsy, and two other NE carcinomas, Merkel Cell Carcinoma (MCC) and small-cell lung cancer (SCLC). We performed cross-tumor comparisons to identify conserved patterns of expression of druggable targets. We tested inhibitors to highly upregulated drug targets in a panel of PC cell lines and in vivo patient-derived xenograft (PDX) models.
- Results: We identified BCL2 as highly upregulated in SCNPC compared to ARPC. Inhibitors targeting BCL2 induced apoptotic cell death in SCNPC cell lines at nanomolar concentrations while ARPC cell lines were resistant. Treatment with the BCL2 inhibitor Navitoclax lead to a reduction of growth of SCNPC PDX tumors in vivo, while ARPC PDX models were more resistant. We identified Wee1 as a second druggable target upregulated in SCNPC. Treatment with the combination of Navitoclax and the Wee1 inhibitor AZD-1775 repressed the growth of SCNPC PDX resistant to single agent BCL2 inhibitors.
- Conclusions: The combination of BCL2 and Wee1 inhibition presents a novel therapeutic strategy for the treatment of SCNPC.
Imaging of Merkel Cell Carcinoma: What Imaging Experts Should Know
Akaike G, Akaike T, Fadl SA, Lachance K, Nghiem P, Behnia F
Radiographics. 2019 Nov-Dec;39(7):2069-2084. doi: 10.1148/rg.2019190102.
PMID: 31697628
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a rare and aggressive cutaneous neuroendocrine tumor with a higher mortality rate than melanoma. Approximately 40% of MCC patients have nodal or distant metastasis at initial presentation, and one-third of patients will develop distant metastatic disease over their clinical course. Although MCC is rare, its incidence has been steadily increasing. Furthermore, the immunogenicity of MCC and its diagnostic and therapeutic application have made MCC one of the most rapidly developing topics in dermatology and oncology. Owing to the aggressive and complex nature of MCC, a multidisciplinary approach is necessary for management of this tumor, including dermatologists, surgeons, radiation oncologists, medical oncologists, pathologists, radiologists, and nuclear medicine physicians. Imaging plays a crucial role in diagnosis, planning for surgery or radiation therapy, and assessment of treatment response and surveillance. However, MCC is still not well recognized among radiologists and nuclear medicine physicians, likely owing to its rarity. The purpose of this review is to raise awareness of MCC among imaging experts by describing the epidemiology, pathophysiology, and clinical features of MCC and current clinical management with a focus on the role of imaging. The authors highlight imaging findings characteristic of MCC, as well as the clinical significance of CT, MRI, sentinel lymph node mapping, fluorine 18 fluorodeoxyglucose PET/CT, and other nuclear medicine studies such as bone scintigraphy and somatostatin receptor scintigraphy.
Less Toxic, More Effective Treatment—A Win-Win for Patients With Merkel Cell Carcinoma
Nghiem P, Park SY
JAMA Dermatol. 2019 Sep 4. doi: 10.1001/jamadermatol.2019.2584.
PMID: 31483436
Abstract and Highlights
- Merkel cell carcinoma (MCC) is an aggressive skin cancer that recurs in more than one-third of cases, with reported mortality rates of 33% to 46%.1 Given this high-risk situation, MCC is often managed with therapies that are aggressive and potentially toxic: extensive surgery, radiation therapy (RT), and systemic therapy. Fortunately, recent advances in multiple realms now allow MCC management to be more effective and less toxic. In this Viewpoint, we highlight 3 recent developments relating to progress in local management, early detection of recurrent disease, and systemic therapy. Although it is not practical for physicians who rarely see patients with MCC to remain up-to-date on the details of management, herein we provide resources and guidelines to help physicians ensure optimal initial care and participate in longitudinal treatment of patients with MCC.
Human CD4+ T Cells Specific for Merkel Cell Polyomavirus Localize to Merkel Cell Carcinomas and Target a Required Oncogenic Domain
Longino NV, Yang J, Iyer JG, Ibrani D, Chow IT, Laing KJ, Campbell VL, Paulson KG, Kulikauskas RM, Church CD, James EA, Nghiem P, Kwok WW, Koelle DM
Cancer Immunol Res. 2019 Oct;7(10):1727-1739. doi: 10.1158/2326-6066.CIR-19-0103.
PMID: 31405946
Abstract and Highlights
- Although CD4+ T cells likely play key roles in antitumor immune responses, most immuno-oncology studies have been limited to CD8+ T-cell responses due to multiple technical barriers and a lack of shared antigens across patients. Merkel cell carcinoma (MCC) is an aggressive skin cancer caused by Merkel cell polyomavirus (MCPyV) oncoproteins in 80% of cases. Because MCPyV oncoproteins are shared across most patients with MCC, it is unusually feasible to identify, characterize, and potentially augment tumor-specific CD4+ T cells. Here, we report the identification of CD4+ T-cell responses against six MCPyV epitopes, one of which included a conserved, essential viral oncogenic domain that binds/disables the cellular retinoblastoma (Rb) tumor suppressor. We found that this epitope (WEDLT209-228) could be presented by three population-prevalent HLA class II alleles, making it a relevant target in 64% of virus-positive MCC patients. Cellular staining with a WEDLT209-228-HLA-DRB1*0401 tetramer indicated that specific CD4+ T cells were detectable in 78% (14 of 18) of evaluable MCC patients, were 250-fold enriched within MCC tumors relative to peripheral blood, and had diverse T-cell receptor sequences. We also identified a modification of this domain that still allowed recognition by these CD4+ T cells but disabled binding to the Rb tumor suppressor, a key step in the detoxification of a possible therapeutic vaccine. The use of these new tools for deeper study of MCPyV-specific CD4+ T cells may provide broader insight into cancer-specific CD4+ T-cell responses.
Treatment Patterns, Overall Survival, and Total Healthcare Costs of Advanced Merkel Cell Carcinoma in the USA
Steuten L, Garmo V, Phatak H, Sullivan SD, Nghiem P, Ramsey SD.
Appl Health Econ Health Policy. 2019 Jun 28. doi: 10.1007/s40258-019-00492-5. [Epub ahead of print]
PMID: 31250217
Abstract and Highlights
- BACKGROUND: Merkel cell carcinoma (MCC) is a rare and aggressive type of cancer with poor outcomes.
- OBJECTIVE: To describe treatment patterns, overall survival, and healthcare costs associated with advanced MCC (aMCC) using data from Medicare enrollees who received an aMCC diagnosis in the USA States between 2006 and 2013.
- METHODS: Surveillance, Epidemiology, and End Results (SEER)-Medicare data from 2006 to 2013 were used to describe treatment patterns, 1- and 5-year overall survival, and total healthcare costs for the periods 12 months before aMCC diagnosis and 4-12 months afterward in patients aged ≥ 65 years.
- RESULTS: We identified 257 patients with an aMCC diagnosis, of whom 51% had stage IIIb disease and 49% had stage IV. Within 4 months after diagnosis, 84% of patients (n = 216) received treatment; 45% (n = 115) received surgery, 48% (n = 124) radiation therapy, and 31% (n = 80) chemotherapy. Second-line chemotherapy was administered in 33% of patients (n = 26) receiving first-line chemotherapy. Median overall survival was 27 months in patients whose aMCC was diagnosed at stage IIIb and 12 months in patients whose aMCC was diagnosed at stage IV. Median total 12-month direct healthcare costs were US$48,006 (25th-75th percentile range = US$30,594-US$69,797) per patient. Total costs were highest in patients receiving chemotherapy, either alone or combined with radiation and/or surgery (US$52,854; 25th-75th percentile range = US$34,473-US$71,987).
- CONCLUSION: Most patients with aMCC received initial treatment, including surgery, radiation, and/or chemotherapy, and approximately one-third of those receiving chemotherapy received second-line chemotherapy. Total 12-month direct healthcare costs were highest in patients who received chemotherapy alone or combined with radiation and/or surgery. These poor survival results and high treatment costs highlight the need for effective new aMCC therapies.
One in a hundred million: Merkel cell carcinoma in pediatric and young adult patients is rare but more likely to present at advanced stages based on US registry data.
Paulson K, Nghiem P
J Am Acad Dermatol. 2019 Jun;80(6):1758-1760. doi: 10.1016/j.jaad.2018.08.021.
PMID: 30165170
Abstract and Highlights
- Published data for pediatric and young adult patients with Merkel cell carcinoma (MCC) are scarce. Case reports from the United States and Europe suggest that MCC can occur in young persons and may be more aggressive in this setting. We sought to determine the frequency of MCC in pediatric and young adult populations and establish whether MCC is more likely to present at advanced stages in younger people. To minimize referral bias and maximize available data, we used the National Program of Cancer Registries Surveillance Epidemiology and End Results (NPCR SEER) database, which captures incident cancer cases in more than 98% of the US population.
Travel burden associated with rare cancers: The example of Merkel cell carcinoma.
Jain R, Menzin J, Lachance K, McBee P, Phatak H, Nghiem PT.
Cancer Med. 2019 May;8(5):2580-2586. doi: 10.1002/cam4.2085. Epub 2019 Apr 5.
PMID: 30950224
Abstract and Highlights
- Background: There are limited data on the travel burden for cancer patients with rare tumor types, such as Merkel cell carcinoma (MCC).
- Objective: The objective of this study was to understand the travel burden of MCC patients.
- Methods: This study used data from an MCC registry at the Seattle Cancer Care Alliance (SCCA). All MCC patients enrolled at SCCA with a valid 3-digit ZIP code were included. Patients were followed up from January 1, 2012 until their last follow-up, death, or end of data (January 1, 2017). Travel burden was measured by one-way travel distance to SCCA from each patient’s 3-digit ZIP code. Patient demographics, tumor characteristics, and follow-up visit were evaluated and stratified by one-way driving distance of ≤300 and >300 miles.
- Results: A total of 391 MCC patients were included (68% men, mean age = 67 years [±SD = ±11 years], 67% residing in the West, and 70% white). At diagnosis, 53% of the patients had Stage III or IV MCC. Mean one-way distance traveled by patients was 1,137 (median: 813) miles, and 57% of patients traveled >300 miles. Compared to patients who traveled ≤300 miles, those who traveled >300 miles were more likely to be <70 years old (46% vs 65%; P < 0.001), were diagnosed with advanced stage (III or IV) MCC (46% vs 59%; P = 0.01), had shorter follow-up in the cancer registry (mean: 509 vs 212 days; P < 0.001), and had fewer visits during follow-up (mean: 5.2 vs 2.5; P < 0.001).
- Conclusions: In this single cancer center study, the majority of MCC patients trav-eled long distances to receive expert care. Longer travel distances appeared to be associated with younger age, a more advanced stage of cancer at study entry and fewer in-clinic visits, suggesting that travel burden may impact timely and adequate patient care for this rare cancer.
Durable Tumor Regression and Overall Survival in Patients With Advanced Merkel Cell Carcinoma Receiving Pembrolizumab as First-Line Therapy.
Nghiem P, Bhatia S, Lipson EJ, Sharfman WH, Kudchadkar RR, Brohl AS, Friedlander PA, Daud A, Kluger HM, Reddy SA, Boulmay BC, Riker AI, Burgess MA, Hanks BA, Olencki T, Margolin K, Lundgren LM, Soni A, Ramchurren N, Church C, Park SY, Shinohara MM, Salim B, Taube JM, Bird SR, Ibrahim N, Fling SP, Homet Moreno B, Sharon E, Cheever MA, Topalian SL.
J Clin Oncol. 2019 Mar 20;37(9):693-702. doi: 10.1200/JCO.18.01896. Epub 2019 Feb 6.
PMID: 30726175
Abstract and Highlights
- Purpose: Merkel cell carcinoma (MCC) is an aggressive skin cancer often caused by the Merkel cell polyomavirus. Clinical trials of programmed cell death-1 pathway inhibitors for advanced MCC (aMCC) demonstrate increased progression-free survival (PFS) compared with historical chemotherapy data. However, response durability and overall survival (OS) data are limited.
- Methods: In this multicenter phase II trial (Cancer Immunotherapy Trials Network-09/Keynote-017), 50 adults naïve to systemic therapy for aMCC received pembrolizumab (2 mg/kg every 3 weeks) for up to 2 years. Radiographic responses were assessed centrally per Response Evaluation Criteria in Solid Tumors (RECIST) v1.1.
- Results: Among 50 patients, the median age was 70.5 years, and 64% had Merkel cell polyomavirus-positive tumors. The objective response rate (ORR) to pembrolizumab was 56% (complete response [24%] plus partial response [32%]; 95% CI, 41.3% to 70.0%), with ORRs of 59% in virus-positive and 53% in virus-negative tumors. Median follow-up time was 14.9 months (range, 0.4 to 36.4+ months). Among 28 responders, median response duration was not reached (range, 5.9 to 34.5+ months). The 24-month PFS rate was 48.3%, and median PFS time was 16.8 months (95% CI, 4.6 months to not estimable). The 24-month OS rate was 68.7%, and median OS time was not reached. Although tumor viral status did not correlate with ORR, PFS, or OS, there was a trend toward improved PFS and OS in patients with programmed death ligand-1-positive tumors. Grade 3 or greater treatment-related adverse events occurred in 14 (28%) of 50 patients and led to treatment discontinuation in seven (14%) of 50 patients, including one treatment-related death.
- Conclusion: Here, we present the longest observation to date of patients with aMCC receiving first-line anti-programmed cell death-1 therapy. Pembrolizumab demonstrated durable tumor control, a generally manageable safety profile, and favorable OS compared with historical data from patients treated with first-line chemotherapy.
Early objective response to avelumab treatment is associated with improved overall survival in patients with metastatic Merkel cell carcinoma.
D'Angelo SP, Hunger M, Brohl AS, Nghiem P, Bhatia S, Hamid O, Mehnert JM, Terheyden P, Shih KC, Brownell I, Lebbé C, Lewis KD, Linette GP, Milella M, Schlichting M, Hennessy MH, Bharmal M.
Cancer Immunol Immunother. 2019 Apr;68(4):609-618. doi: 10.1007/s00262-018-02295-4. Epub 2019 Feb 5.
PMID: 30721341
Abstract and Highlights
- Background: Response rates are primary endpoints in many oncology trials; however, correlation with overall survival (OS) is not uniform across cancer types, treatments, or lines of therapy. This study explored the association between objective response (OR) and OS in patients with chemotherapy-refractory metastatic Merkel cell carcinoma who received avelumab (anti-PD-L1).
- Methods: Eighty-eight patients enrolled in JAVELIN Merkel 200 (part A; NCT02155647) received i.v. avelumab 10 mg/kg every 2 weeks until confirmed progression, unacceptable toxicity, or withdrawal. Using conditional landmark analyses, we compared OS in patients with and without confirmed OR (RECIST v1.1). We applied a Cox model that included OR as a time-varying covariate and adjusted for age, visceral disease, and number of previous therapies.
- Results: Twenty-nine patients had confirmed OR; 20 by study week 7 and 7 more between study weeks 7 and 13. Survival probabilities 18 months after treatment initiation were 90% [95% confidence interval (CI) 65.6-97.4] in patients with OR at week 7 and 26.2% (95% CI 15.7-37.8) in patients without OR but who were alive at week 7. Median OS was not reached in patients with OR and was 8.8 months (95% CI 6.4-12.9) in patients without. Similar results were observed for the week 13 landmark. The adjusted Cox model showed OR was associated with a 95% risk reduction of death [hazard ratio 0.052 (95% CI 0.018-0.152)] compared with a non-response.
- Conclusions: Patients with OR by 7 or 13 weeks had significantly longer OS than patients without, confirming that early OR is an endpoint of major importance.
Tuberculosis following PD-1 blockade for cancer immunotherapy
Barber DL, Sakai S, Kudchadkar RR, Fling SP, Day TA, Vergara JA, Ashkin D, Cheng JH, Lundgren LM, Raabe VN, Kraft CS, Nieva JJ, Cheever MA, Nghiem PT, Sharon E
Sci Transl Med. 2019 Jan 16;11(475). pii: eaat2702. doi: 10.1126/scitranslmed.aat2702.
PMID: 30651320
Abstract and Highlights
- Because of the well-established therapeutic benefit of boosting antitumor responses through blockade of the T cell inhibitory receptor PD-1, it has been proposed that PD-1 blockade could also be useful in infectious disease settings, including Mycobacterium tuberculosis (Mtb) infection. However, in preclinical models, Mtb-infected PD-1-/- mice mount exaggerated TH1 responses that drive lethal immunopathology. Multiple cases of tuberculosis during PD-1 blockade have been observed in patients with cancer, but in humans little is understood about Mtb-specific immune responses during checkpoint blockade-associated tuberculosis. Here, we report two more cases. We describe a patient who succumbed to disseminated tuberculosis after PD-1 blockade for treatment of nasopharyngeal carcinoma, and we examine Mtb-specific immune responses in a patient with Merkel cell carcinoma who developed checkpoint blockade-associated tuberculosis and was successfully treated for the infection. After anti-PD-1 administration, interferon-γ-producing Mtb-specific CD4 T cells became more prevalent in the blood, and a tuberculoma developed a few months thereafter. Mtb-specific TH17 cells, CD8 T cells, regulatory T cells, and antibody abundance did not change before the appearance of the granuloma. These results are consistent with the murine model data and suggest that boosting TH1 function with PD-1 blockade may increase the risk or severity of tuberculosis in humans.
Differential Outcomes Among Immunosuppressed Patients With Merkel Cell Carcinoma: Impact of Immunosuppression Type on Cancer-specific and Overall Survival.
Cook M, Baker K, Redman M, Lachance K, Nguyen MH, Parvathaneni U, Bhatia S, Nghiem P, Tseng YD.
Am J Clin Oncol. 2019 Jan;42(1):82-88. doi: 10.1097/COC.0000000000000482.
PMID: 30211723
Abstract and Highlights
- Objectives: Merkel cell carcinoma (MCC) is a rare, aggressive neuroendocrine skin cancer with higher incidence among whites, elderly, and immunosuppressed patients. Although immunosuppressed MCC patients are at higher risk of recurrence and MCC-related death, it is unknown whether immunosuppression type is associated with differential outcomes.
- Methods: We retrospectively evaluated 89 nonmetastatic MCC patients with a diagnosis of chronic immunosuppression. Immunosuppression was categorized as chronic lymphocytic leukemia (31% of cohort), other hematologic malignancies (18%), solid organ transplant (21%), autoimmune disease (21%), and human immunodeficiency virus acquired deficiency syndrome (8%). Progression-free survival (PFS) and MCC-specific survival (MSS) were estimated with the cumulative incidence function. Overall survival (OS) was estimated by the Kaplan-Meier method.
- Results: With a median follow-up of 52 months, 53 deaths occurred (42 from MCC, 7 unknown, and 4 non-MCC). Two-year PFS, MSS, and OS were 30%, 55%, and 52%, respectively. Human immunodeficiency virus/acquired deficiency syndrome and solid organ transplant patients were diagnosed with MCC at a younger age (median 55 and 59 y, respectively) and with more advanced stage disease compared with other immunosuppressed subgroups. PFS did not significantly differ among the 5 immunosuppression subgroups (P=0.30), but significant differences were observed in MSS and OS (both P=0.01). Controlling for potential confounders for OS, including age and stage, immunosuppression type was still significantly associated with risk of death (P=0.01).
- Conclusions: Among immunosuppressed MCC patients, recurrent MCC is the major cause of mortality. The risk of death from MCC differs among immunosuppression types, suggesting important biological differences in host-tumor immune interactions.
2018
The biology and treatment of Merkel cell carcinoma: current understanding and research priorities.
Harms PW, Harms KL, Moore PS, DeCaprio JA, Nghiem P, Wong MKK, Brownell I
Nat Rev Clin Oncol. 2018 Dec;15(12):763-776. doi: 10.1038/s41571-018-0103-2.
PMID: 30287935
Abstracts and Highlights
- Merkel cell carcinoma (MCC) is a rare and aggressive skin cancer associated with advanced age and immunosuppression. Over the past decade, an association has been discovered between MCC and either integration of the Merkel cell polyomavirus, which likely drives tumorigenesis, or somatic mutations owing to ultraviolet-induced DNA damage. Both virus-positive and virus-negative MCCs are immunogenic, and inhibition of the programmed cell death protein 1 (PD-1)-programmed cell death 1 ligand 1 (PD-L1) immune checkpoint has proved to be highly effective in treating patients with metastatic MCC; however, not all patients have a durable response to immunotherapy. Despite these rapid advances in the understanding and management of patients with MCC, many basic, translational and clinical research questions remain unanswered. In March 2018, an International Workshop on Merkel Cell Carcinoma Research was held at the US National Cancer Institute, at which academic, government and industry experts met to identify the highest-priority research questions. Here, we review the biology and treatment of MCC and report the consensus-based recommendations agreed upon during the workshop.
Merkel cell polyomavirus-specific immune responses in patients with Merkel cell carcinoma receiving anti-PD-1 therapy
Miller N, Church C, Fling S, Kulikauskas R, Ramchurren N, Shinohara M, Kluger H, Bhatia S, Lundgren L, Cheever M, Topalian S, Nghiem P
J Immunother Cancer. 2018 Nov 27;6(1):131. doi: 10.1186/s40425-018-0450-7.
PMID: 30482247
View Abstract and Highlights
- Background: Merkel cell carcinoma (MCC) is an aggressive skin cancer that frequently responds to anti-PD-1 therapy. MCC is associated with sun exposure and, in 80% of cases, Merkel cell polyomavirus (MCPyV). MCPyVspecific T and B cell responses provide a unique opportunity to study cancer-specific immunity throughout PD-1 blockade therapy.
- Methods: Immune responses were assessed in patients (n = 26) with advanced MCC receiving pembrolizumab. Peripheral blood mononuclear cells (PBMC) were collected at baseline and throughout treatment. MCPyVoncoprotein antibodies were quantified and T cells were assessed for MCPyV-specificity via tetramer staining and/or cytokine secretion. Pre-treatment tumor biopsies were analyzed for T cell receptor clonality.
- Results: MCPyV oncoprotein antibodies were detectable in 15 of 17 (88%) of virus-positive MCC (VP-MCC) patients. Antibodies decreased in 10 of 11 (91%) patients with responding tumors. Virus-specific T cells decreased over time in patients who had a complete response, and increased in patients who had persistent disease. Tumors that were MCPyV(+) had a strikingly more clonal (less diverse) intratumoral TCR repertoire than virus-negative tumors (p = 0.0001).
- Conclusions: Cancer-specific T and B cell responses generally track with disease burden during PD-1 blockade, in proportion to presence of antigen. Intratumoral TCR clonality was significantly greater in VP-MCC than VN-MCC tumors, suggesting expansion of a limited number of dominant clones in response to fewer immunogenic MCPyV antigens. In contrast, VN-MCC tumors had lower clonality, suggesting a diverse T cell response to numerous neoantigens. These findings reveal differences in tumor-specific immunity for VP-MCC and VN-MCC, both of which often respond to anti- PD-1 therapy.
- Keywords: Merkel cell carcinoma, Merkel cell polyomavirus, Viral cancer antigen, Immunotherapy, Pembrolizumab,
- Anti-PD-1, T cell
T cell receptor fingerprinting enables in-depth characterization of the interactions governing recognition of peptide–MHC complexes
Bentzen A, Such L, Jensen K, Marquard A, Jessen L, Miller N, Church C, Lyngaa R, Koelle D, Becker J, Linnemann C, Schumacher T, Marcatili P, Nghiem P, Nielsen M, Hadrup S
Nat Biotechnol. 2018 Nov 19. doi: 10.1038/nbt.4303.
PMID: 30451992
Abstract and Highlights
- The promiscuous nature of T-cell receptors (TCRs) allows T cells to recognize a large variety of pathogens, but makes it challenging to understand and control T-cell recognition1. Existing technologies provide limited information about the key requirements for T-cell recognition and the ability of TCRs to cross-recognize structurally related elements2,3. Here we present a ‘one-pot’ strategy for determining the interactions that govern TCR recognition of peptide–major histocompatibility complex (pMHC). We measured the relative affinities of TCRs to libraries of barcoded peptide–MHC variants and applied this knowledge to understand the recognition motif, here termed the TCR fingerprint. The TCR fingerprints of 16 different TCRs were identified and used to predict and validate cross-recognized peptides from the human proteome. The identified fingerprints differed among TCRs recognizing the same epitope, demonstrating the value of this strategy for understanding T-cell interactions and assessing potential cross-recognition before selection of TCRs for clinical development.
Multidimensional, quantitative assessment of PD-1/PD-L1 expression in patients with Merkel cell carcinoma and association with response to pembrolizumab.
Giraldo NA, Nguyen P, Engle EL, Kaunitz GJ, Cottrell TR, Berry S, Green B, Soni A, Cuda JD, Stein JE, Sunshine JC, Succaria F, Xu H, Ogurtsova A, Danilova L, Church CD, Miller NJ, Fling S, Lundgren L, Ramchurren N, Yearley JH, Lipson EJ, Cheever M, Anders RA, Nghiem PT, Topalian SL, Taube JM
J Immunother Cancer. 2018 Oct 1;6(1):99. doi: 10.1186/s40425-018-0404-0.
PMID: 30285852
Abstract and Highlights
- Background: We recently reported a 56% objective response rate in patients with advanced Merkel cell carcinoma (MCC) receiving pembrolizumab. However, a biomarker predicting clinical response was not identified.
- Methods: Pretreatment FFPE tumor specimens (n = 26) were stained for CD8, PD-L1, and PD-1 by immunohistochemistry/immunofluorescence (IHC/IF), and the density and distribution of positive cells was quantified to determine the associations with anti-PD-1 response. Multiplex IF was used to test a separate cohort of MCC archival specimens (n = 16), to identify cell types expressing PD-1.
- Results: Tumors from patients who responded to anti-PD-1 showed higher densities of PD-1+ and PD-L1+ cells when compared to non-responders (median cells/mm2, 70.7 vs. 6.7, p = 0.03; and 855.4 vs. 245.0, p = 0.02, respectively). There was no significant association of CD8+ cell density with clinical response. Quantification of PD-1+ cells located within 20 μm of a PD-L1+ cell showed that PD-1/PD-L1 proximity was associated with clinical response (p = 0.03), but CD8/PD-L1 proximity was not. CD4+ and CD8+ cells in the TME expressed similar amounts of PD-1.
- Conclusions: While the binomial presence or absence of PD-L1 expression in the TME was not sufficient to predict response to anti-PD-1 in patients with MCC, we show that quantitative assessments of PD-1+ and PD-L1+ cell densities as well as the geographic interactions between these two cell populations correlate with clinical response. Cell types expressing PD-1 in the TME include CD8+ T-cells, CD4+ T-cells, Tregs, and CD20+ B-cells, supporting the notion that multiple cell types may potentiate tumor regression following PD-1 blockade.
Acquired cancer resistance to combination immunotherapy from transcriptional loss of class I HLA.
Paulson KG, Voillet V, McAfee MS, Hunter DS, Wagener FD, Perdicchio M, Valente WJ, Koelle SJ, Church CD, Vandeven N, Thomas H, Colunga AG, Iyer JG, Yee C, Kulikauskas R, Koelle DM, Pierce RH, Bielas JH, Greenberg PD, Bhatia S, Gottardo R, Nghiem P, Chapuis AG.
Nat Commun. 2018 Sep 24;9(1):3868. doi: 10.1038/s41467-018-06300-3.
PMID: 30250229
Abstract and Highlights
- Understanding mechanisms of late/acquired cancer immunotherapy resistance is critical to improve outcomes; cellular immunotherapy trials offer a means to probe complex tumor-immune interfaces through defined T cell/antigen interactions. We treated two patients with metastatic Merkel cell carcinoma with autologous Merkel cell polyomavirus specific CD8+ T cells and immune-checkpoint inhibitors. In both cases, dramatic remissions were associated with dense infiltration of activated CD8+s into the regressing tumors. However, late relapses developed at 22 and 18 months, respectively. Here we report single cell RNA sequencing identified dynamic transcriptional suppression of the specific HLA genes presenting the targeted viral epitope in the resistant tumor as a consequence of intense CD8-mediated immunologic pressure; this is distinguished from genetic HLA-loss by its reversibility with drugs. Transcriptional suppression of Class I loci may underlie resistance to other immunotherapies, including checkpoint inhibitors, and have implications for the design of improved immunotherapy treatments.
Bhatia S, Miller NJ, Lu H, Vandeven NV, Ibrani D, Shinohara M, Byrd D, Parvathaneni U, Kulikauskas RM, Ter Meulen J, Hsu FJ, Koelle DM, Nghiem P
Clin Cancer Res. 2018 Aug 9. pii: clincanres.0469.2018.
PMID: 30093453
Abstract and Highlights
- PURPOSE: G100 is a toll-like receptor 4 (TLR4) agonist that triggers innate and adaptive anti-tumor immune responses in preclinical models. This pilot study assessed the safety, efficacy, and immunologic activity of intratumoral (IT) administration of G100 in patients with Merkel cell carcinoma (MCC).
- EXPERIMENTAL DESIGN: Patients with loco-regional MCC (n=3; Cohort A) received neoadjuvant IT G100 (2 weekly doses at 5 μg/dose) followed by surgery and radiotherapy; patients with metastatic MCC (n=7; Cohort B) received 3 doses in a 6-week cycle and could receive additional cycles with/without radiotherapy.
- RESULTS: IT G100 was safe and feasible in both neoadjuvant and metastatic settings. Treatment-related adverse events were mostly grade 1 or 2 injection site reactions. IT G100 led to increased inflammation in the injected tumors with infiltration of CD8+and CD4+T cells and activation of immune-related genes. These pro-inflammatory changes were associated with local tumor regression and appeared to promote systemic immunity. All 3 Cohort A patients successfully completed therapy; 2 patients remain recurrence-free at 44+ and 41+ months, including one with a pathologic complete response after G100 alone. In Cohort B, 2 patients achieved sustained partial responses, both lasting 33+ months after 2 cycles of therapy.
- CONCLUSIONS: In this first-in-human study, IT G100 induced anti-tumor immune responses, demonstrated acceptable safety, and showed encouraging clinical activity.
Gavvovidis I, Leisegang M, Willimsky G, Miller NJ, Nghiem P, Blankenstein T.
Clin Cancer Res. 2018 Aug 1;24(15):3644-3655.
PMID: 29669806
Abstract and Highlights
- Purpose: The causative agent of most cases of Merkel cell carcinoma (MCC) has been identified as the Merkel cell polyomavirus (MCV). MCV-encoded T antigens (Tag) are essential not only for virus-mediated tumorigenesis but also for maintaining MCC cell lines in vitro MCV Tags are thus an appealing target for viral oncoprotein-directed T-cell therapy for MCC. With this study, we aimed to isolate and characterize Tag-specific T-cell receptors (TCR) for potential use in gene therapy clinical trials.Experimental Design: T-cell responses against MCV Tag epitopes were investigated by immunizing transgenic mice that express a diverse human TCR repertoire restricted to HLA-A2. Human lymphocytes genetically engineered to express Tag-specific TCRs were tested for specific reactivity against MCC cell lines. The therapeutic potential of Tag-specific TCR gene therapy was tested in a syngeneic cancer model.Results: We identified naturally processed epitopes of MCV Tags and isolated Tag-specific TCRs. T cells expressing these TCRs were activated by HLA-A2-positive cells loaded with cognate peptide or cells that stably expressed MCV Tags. We showed cytotoxic potential of T cells engineered to express these TCRs in vitro and demonstrated regression of established tumors in a mouse model upon TCR gene therapy.
- Conclusions: Our findings demonstrate that MCC cells can be targeted by MCV Tag-specific TCRs. Although recent findings suggest that approximately half of MCC patients benefit from PD-1 pathway blockade, additional patients may benefit if their endogenous T-cell response can be augmented by infusion of transgenic MCV-specific T cells such as those described here. Clin Cancer Res; 24(15); 3644-55. ©2018 AACR.
Circulating cell-free miR-375 as surrogate marker of tumor burden in Merkel cell carcinoma.
Kaiji Fan, Cathrin Ritter, Paul Nghiem, Astrid Blom, Monique E Verhaegen, Andrzej Dlugosz, Niels Odum, Anders Woetmann, Richard W. Tothill, Rodney J. Hicks, Michael Sand, David Schrama, Dirk Schadendorf, Selma Ugurel and Jurgen C Becker
Clin Cancer Res 2018
PMID: 30061360
Abstract and Highlights
- Purpose: Merkel cell carcinoma (MCC) is an aggressive skin cancer with neuroendocrine differentiation. There is an unmet need for MCC-specific blood-based surrogate biomarkers of tumor burden; circulating cell-free micro(mi)RNA may serve this purpose. Experimental Design: Expression of miR-375 was quantified in 24 MCC and 23 non-MCC cell lines, 67 MCC and 58 non-MCC tumor tissues, sera of two preclinical MCC models, sera of 109 MCC patients and 30 healthy controls by nCounter®human-v2-miRNA expression or miR-375 specific real-time PCR assays. The patients’ sera consisted of two retrospective (discovery and training) and two prospective (validation) cohorts. Results: miR-375 expression was high in MCC cell lines and tissues compared to non-MCCs. It was readily detected in MCC conditioned medium and sera of preclinical models bearing MCC xenografts. miR-375 levels were higher in sera from tumor-bearing MCC patients than in tumor-free patients or healthy controls (p<0.0005). Moreover, miR-375 serum levels correlated with tumor stage in tumor-bearing (p=0.037) but not in tumor-free (p=0.372) MCC patients. miR-375 serum level showed high diagnostic accuracy to discriminate tumor-bearing and tumor-free MCC patients as demonstrated by receiver operating characteristic curve analysis in the retrospective cohorts (AUC=0.954 and 0.800) as well as in the prospective cohorts (AUC=0.929 and 0.959). miR-375 serum level reflected dynamic changes in tumor burden of MCC patients during therapeutic interventions. Conclusions: Circulating cell-free miR-375 proved as a surrogate marker for tumor burden in MCC without restriction to polyomavirus positivity, it thus appears to be useful for therapy monitoring and the follow-up of MCC patients.
Merkel Cell Carcinoma, Version 1.2018, NCCN Clinical Practice Guidelines in Oncology.
Bichakjian CK, Olencki T, Aasi SZ, Alam M, Andersen JS, Blitzblau R, Bowen GM, Contreras CM, Daniels GA, Decker R, Farma JM, Fisher K, Gastman B, Ghosh K, Grekin RC, Grossman K, Ho AL, Lewis KD, Loss M, Lydiatt DD, Messina J, Nehal KS, Nghiem P, Puzanov I, Schmults CD, Shaha AR, Thomas V, Xu YG, Zic JA, Hoffmann KG, Engh AM.
J Natl Compr Canc Netw. 2018 Jun;16(6):742-774
PMID: 29891526
Abstract and Highlights
- This selection from the NCCN Guidelines for Merkel Cell Carcinoma (MCC) focuses on areas impacted by recently emerging data, including sections describing MCC risk factors, diagnosis, workup, follow-up, and management of advanced disease with radiation and systemic therapy. Included in these sections are discussion of the new recommendations for use of Merkel cell polyomavirus as a biomarker and new recommendations for use of checkpoint immunotherapies to treat metastatic or unresectable disease. The next update of the complete version of the NCCN Guidelines for MCC will include more detailed information about elements of pathology and addresses additional aspects of management of MCC, including surgical management of the primary tumor and draining nodal basin, radiation therapy as primary treatment, and management of recurrence.
Effect of Patient Immune Status on the Efficacy of Radiation Therapy and Recurrence-Free Survival Among 805 Patients With Merkel Cell Carcinoma.
Tseng YD, Nguyen MH, Baker K, Cook M, Redman M, Lachance K, Bhatia S, Liao JJ, Apisarnthanarax S, Nghiem PT, Parvathaneni U.
Int J Radiat Oncol Biol Phys. 2018 Oct 1;102(2):330-339. doi: 10.1016/j.ijrobp.2018.05.075. Epub 2018 Jun 5.
PMID: 30191867
Abstract and Highlights
- Purpose: Patients with Merkel cell carcinoma (MCC) with chronic immunosuppression (IS) have worse outcomes, but the mechanisms are not well understood. We hypothesized that these differences may be mediated in part by differential response to treatment, and we evaluated whether radiation therapy (RT) efficacy is altered among IS compared with immune-competent (IC) patients with MCC.
- Methods: Among 805 patients with MCC, recurrence-free survival (RFS) and patterns of first recurrence were compared between 89 IS and 716 IC patients with stage I to III MCC treated with curative intent. We used a Fine and Gray’s competing risk multivariable analysis to estimate associations with RFS.
- Results: IS and IC patients with MCC had similar demographic and disease characteristics. Most (77% IC, 86% IS) were irradiated (median, 50.4 Gy IC, 50.3 Gy IS), although more IS patients were irradiated to the primary site (97% vs 81%). With a median follow-up of 54.4 months, IS patients had inferior RFS (2-year: 30% vs 57%; P < .0001) and higher rates of local recurrence as the first site of relapse (25% vs 12%; P = .0002). The association between RT and RFS differed by immune status (interaction P = .01). Although RT was associated with significantly improved RFS among IC patients (hazard ratio 0.56, 95% confidence interval 0.44-0.72), no difference in RFS was observed with RT among IS patients (hazard ratio 1.49, 95% confidence interval 0.70-3.17).=
- Conclusions: Radiation therapy efficacy at current standard RT doses for MCC is impaired among immunosuppressed patients with MCC. Although a strong link between durability of RT response and immune function does not appear to be evident in most cancers, our results may reflect an especially dynamic interaction between immune status and RT efficacy in MCC.
The association between geographic location and incidence of Merkel cell carcinoma in comparison to melanoma: An international assessment.
Stang A, Becker JC, Nghiem P, Ferlay J
Eur J Cancer. 2018 May;94:47-60
PMID: 29533867
Abstract and Highlights
- Aim: The aim of this article was to provide worldwide, population-based incidence rates for Merkel cell carcinoma (MCC).
- Methods: We included 11,576 cases from 20 countries for time trend analyses (1990–2007) and 11,028 cases (2.5 billion person-years) from 21 countries for the period 2003–2007 extracted from Cancer Incidence in Five Continents. We computed age-standardised incidence rates (World Standard population) per million person years and sex ratios of these rates. We estimated annual percentage changes (EAPCs) of the incidence and studied the association between geographic latitude and MCC incidence. We examined the body site distribution of MCC.
- Findings: In the majority of populations, the incidence has increased over time (EAPC, men 2.0–21.0%; women 1.6–27.2%). Rate differences between 1995 and 2007 were typically small (men: 0.8–2.2; women: 0.2–1.7). The incidence was relatively stable in some populations (men: U.S. blacks, Japan, Norway, Denmark; women: Denmark, Norway, Sweden). Incidences from 2003 to 2007 were highest in Australia, New Zealand, the United States and Israel among men and in New Zealand, Australia, Ireland and the Netherlands among women. The incidence of MCC and melanoma among white non-Hispanic males in North America was positively associated with living closer to the equator. The proportion of MCC on the head was higher with advanced age. The head was a less likely primary site among blacks as compared with any other ethnicity.
- Interpretation: Several countries showed increases in MCC incidence among white non-Hispanics over time. Latitude closer to the equator was associated with the MCC incidence in North American men, but barely in women, possibly due to occupational sunlight exposure patterns.
Merkel Cell Carcinoma in the Age of Immunotherapy: Facts and Hopes.
Colunga A, Pulliam T, Nghiem P.
Clin Cancer Res. 2018 May 1;24(9):2035-2043.
PMID: 29217527
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a rare (∼2,000 U.S. cases/year) but aggressive neuroendocrine tumor of the skin. For advanced MCC, cytotoxic chemotherapy only infrequently (<10% of cases) offers durable clinical responses (>1 year), suggesting a great need for improved therapeutic options. In 2008, the Merkel cell polyomavirus (MCPyV) was discovered and is clonally integrated in approximately 80% of MCC tumors. The remaining 20% of MCC tumors have large numbers of UV-associated mutations. Importantly, both the UV-induced neoantigens in virus-negative tumors and the MCPyV T antigen oncogenes that are required for virus-positive tumor growth are immunogenic. Indeed, antigen-specific T cells detected in patients are frequently dysfunctional/”exhausted,” and the inhibitory ligand, PD-L1, is often present in MCC tumors. These findings led to recent clinical trials involving PD-1 pathway blockade in advanced MCC. The combined data from these trials involving three PD-1 pathway blocking agents-avelumab, pembrolizumab, and nivolumab-indicated a high frequency of durable responses in treated patients. Of note, prior treatment with chemotherapy was associated with decreased response rates to PD-1 checkpoint blockade. Over the past year, these striking data led to major changes in advanced MCC therapy, including the first-ever FDA drug approval for this disease. Despite these successes, approximately 50% of patients with MCC do not persistently benefit from PD-1 pathway blockade, underscoring the need for novel strategies to broaden antitumor immune responses in these patients. Here, we highlight recent progress in MCC including the underlying mechanisms of immune evasion and emerging approaches to augment the efficacy of PD-1 pathway blockade. Clin Cancer Res; 24(9); 2035-43. ©2017 AACR.
Clinical Benefit from Tyrosine Kinase Inhibitors in Metastatic Merkel Cell Carcinoma: A Case Series of 5 Patients.
Tarabadkar ES, Thomas H, Blom A, Parvathaneni U, Olencki T, Nghiem P, Bhatia S.
Am J Case Rep 2018; 19:505-511
PMID: 29706615
Abstract and Highlights
BACKGROUND: Merkel cell carcinoma (MCC) is a rare but aggressive neuroendocrine skin cancer. The estimated 5-year survival of patients with metastatic disease is approximately 14%. Cytotoxic chemotherapy is associated with a modest median progression-free survival (PFS) of only 3 months. In recent studies, immunotherapy with anti-PD-1/anti-PD-L1 antibodies has demonstrated a high response rate in immunocompetent patients (>50% in chemotherapy-naïve patients) and responses are typically durable. However, approximately 50% of immunocompetent patients do not respond to immunotherapy. In addition, immunosuppressed patients have limited therapeutic options. Hence, there is a significant unmet need for effective treatments in these subpopulations.
CASE REPORT: We describe 5 patients (out of 24 total) with metastatic MCC who were treated with a vascular endothelial growth factor receptor (VEGFR) tyrosine kinase inhibitor (TKI), either pazopanib (n=4) or cabozantinib (n=1), with clinical benefit. One patient had a complete response to pazopanib after 3 months of therapy. Four patients had stabilization of disease that lasted from 5 months to 3.5 years. In an immunosuppressed patient with psoriatic arthritis, stabilization of MCC was also associated with improvement in his arthritis that allowed cessation of immunosuppression. Patients did not develop any unusual toxicities from VEGFR-TKIs.
CONCLUSIONS: Treatment with VEGFR-TKIs demonstrated clinical benefit in this selected small group of patients with metastatic MCC. Prospective investigation of VEGFR-TKIs is warranted in this population, especially in patients with disease refractory to immunotherapy.
Epidemiology, biology and therapy of Merkel cell carcinoma: conclusions from the EU project IMMOMEC.
Becker JC, Stang A, zur Hausen A, Fischer N, DeCaprio JA, Tothill RW, Lyngaa R, Hansen UK, Ritter C, Nghiem P, Bichakjian CK, Ugurel S, Schrama D.
Cancer Immunol Immunother. 2018 Mar;67(3):341-351.
PMID: 29188306
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a highly aggressive, often lethal neuroendocrine cancer. Its carcinogenesis may be either caused by the clonal integration of the Merkel cell polyomavirus into the host genome or by UV-induced mutations. Notably, virally-encoded oncoproteins and UV-induced mutations affect comparable signaling pathways such as RB restriction of cell cycle progression or p53 inactivation. Despite its low incidence, MCC recently received much attention based on its exquisite immunogenicity and the resulting major success of immune modulating therapies. Here, we summarize current knowledge on epidemiology, biology and therapy of MCC as conclusion of the project ‘Immune Modulating strategies for treatment of Merkel Cell Carcinoma’, which was funded over a 5-year period by the European Commission to investigate innovative immunotherapies for MCC.
Merkel cell carcinoma: Current US incidence and projected increases based on changing demographics.
Paulson KG, Park SY, Vandeven NA, Lachance K, Thomas H, Chapuis AG, Harms KL, Thompson JA, Bhatia S, Stang A, Nghiem P.
J Am Acad Dermatol. 2018 Mar;78(3):457-463.
PMID: 29102486
Abstract and Highlights
- BACKGROUND: Merkel cell carcinoma (MCC) incidence rates are rising and strongly age-associated, relevant for an aging population.
- OBJECTIVE: Determine MCC incidence in the United States and project incident cases through the year 2025.
- METHODS: Registry data were obtained from the SEER-18 Database, containing 6600 MCC cases. Age- and sex-adjusted projections were generated using US census data.
- RESULTS: During 2000-2013, the number of reported solid cancer cases increased 15%, melanoma cases increased 57%, and MCC cases increased 95%. In 2013, the MCC incidence rate was 0.7 cases/100,000 person-years in the United States, corresponding to 2488 cases/year. MCC incidence increased exponentially with age, from 0.1 to 1.0 to 9.8 (per 100,000 person-years) among age groups 40-44 years, 60-64 years, and ≥85 years, respectively. Due to aging of the Baby Boomer generation, US MCC incident cases are predicted to climb to 2835 cases/year in 2020 and 3284 cases/year in 2025.
- LIMITATIONS: We assumed that the age-adjusted incidence rate would stabilize, and thus, the number of incident cases we projected might be an underestimate.
- CONCLUSION: An aging population is driving brisk increases in the number of new MCC cases in the United States. This growing impact combined with the rapidly evolving therapeutic landscape warrants expanded awareness of MCC diagnosis and management.
Merkel Cell Carcinoma Patients Presenting Without a Primary Lesion Have Elevated Markers of Immunity, Higher Tumor Mutation Burden, and Improved Survival.
Vandeven N, Lewis CW, Makarov V, Riaz N, Paulson KG, Hippe D, Bestick A, Doumani R, Marx T, Takagishi S, Chan TA, Choi J, Nghiem P.
Clin Cancer Res. 2018 Feb 15;24(4):963-971.
PMID: 29246939
Abstract and Highlights
- Purpose: Patients presenting with nodal Merkel cell carcinoma without an identifiable (unknown) primary lesion (MCC-UP) are nearly twice as likely to survive compared with similarly staged patients with known primary lesions (MCC-KP). The basis of this previously reported finding is unclear.Experimental Design: Survival analyses and markers of immunity were evaluated in 123 patients with advanced MCC. Whole-exome sequence data were analyzed from 16 tumors.Results: As in prior studies, patients with nodal MCC-UP had strikingly improved MCC-specific survival as compared with MCC-KP patients (HR, 0.297; P < 0.001). Surprisingly, patients presenting with distant metastatic MCC-UP also had significantly improved survival (HR, 0.296; P = 0.038). None of the 72 patients with MCC-UP were immunosuppressed as compared to 12 of the 51 (24%) patients with MCC-KP (P < 0.001). Merkel polyomavirus oncoprotein antibody median titer was higher in MCC-UP patients (26,229) than MCC-KP patients (3,492; P < 0.001). In addition, the median number of nonsynonymous exome mutations in MCC-UP tumors (688 mutations) was markedly higher than MCC-KP tumors (10 mutations, P = 0.016).Conclusions: This is the first study to our knowledge to explore potential underlying immune-mediated mechanisms of MCC-UP presentation. In this cohort, MCC-UP patients were never immune suppressed, had higher oncoprotein antibody titers, and higher tumor mutational burdens. In addition, we show that nodal tumors identified in MCC-UP patients did indeed arise from primary skin lesions as they contained abundant UV-signature mutations. These findings suggest that stronger underlying immunity against MCC contributes to primary lesion elimination and improved survival
Updated efficacy of avelumab in patients with previously treate metastatic Merkel cell carcinoma after ≥1 year of follow-up: JAVELIN Merkel 200, a phase 2 clinical trail.
Kaufman HL, Russell JS, Hamid O, Bhatia S, Terheyden P, D’Angelo SP, Shih KC, Lebbé C, Milella M, Brownell I, Lewis KD, Lorch JH, von Heydebreck A, Hennessy M, Nghiem P.
J Immunother Cancer. 2018 Jan 19;6(1):7.
PMID: 29347993
Abstract and Highlights
- BACKGROUND: Merkel cell carcinoma (MCC) is a rare, aggressive skin cancer associated with poor survival outcomes in patients with distant metastatic disease (mMCC). In an initial analysis from JAVELIN Merkel 200, a phase 2, prospective, open-label, single-arm trial in mMCC, avelumab-a human anti-programmed death-ligand 1 (PD-L1) monoclonal antibody-showed promising efficacy and a safety profile that was generally manageable and tolerable. Here, we report the efficacy of avelumab after ≥1 year of follow-up in patients with distant mMCC that had progressed following prior chemotherapy for metastatic disease.
- PATIENTS AND METHODS: Patients received avelumab 10 mg/kg by 1-h intravenous infusion every 2 weeks until confirmed disease progression, unacceptable toxicity, or withdrawal. The primary endpoint was best overall response. Secondary endpoints included duration of response (DOR), progression-free survival (PFS), and overall survival (OS).
- RESULTS: Patients (N = 88) were followed for a minimum of 12 months. The confirmed objective response rate was 33.0% (95% CI, 23.3%-43.8%; complete response: 11.4%). An estimated 74% of responses lasted ≥1 year, and 72.4% of responses were ongoing at data cutoff. Responses were durable, with the median DOR not yet reached (95% CI, 18.0 months-not estimable), and PFS was prolonged; 1-year PFS and OS rates were 30% (95% CI, 21%-41%) and 52% (95% CI, 41%-62%), respectively. Median OS was 12.9 months (95% CI, 7.5-not estimable). Subgroup analyses suggested a higher probability of response in patients receiving fewer prior lines of systemic therapy, with a lower baseline disease burden, and with PD-L1-positive tumors; however, durable responses occurred irrespective of baseline factors, including tumor Merkel cell polyomavirus status.
- CONCLUSIONS: With longer follow-up, avelumab continues to show durable responses and promising survival outcomes in patients with distant mMCC whose disease had progressed after chemotherapy.
2017
Merkel Cell Carcinoma
Becker JC, Stang A, DeCaprio JA, Cerroni L, Lebbé C, Veness M, Nghiem P
Nat Rev Dis Primers. 2017 Oct 26;3:17077.
PMID: 29072302
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a rare but highly aggressive skin cancer with neuroendocrine features. MCC pathogenesis is associated with either the presence of Merkel cell polyomavirus or chronic exposure to ultraviolet light (UV), which can cause a characteristic pattern of multiple DNA mutations. Notably, in the Northern hemisphere, the majority of MCC cases are of viral aetiology; by contrast, in areas with high UV exposure, UV-mediated carcinogenesis is predominant. The two aetiologies share similar clinical, histopathological and prognostic characteristics. MCC presents with a solitary cutaneous or subcutaneous nodule, most frequently in sun-exposed areas. In fact, UV exposure is probably involved in both viral-mediated and non-viral-mediated carcinogenesis, by contributing to immunosuppression or DNA damage, respectively. Confirmation of diagnosis relies on analyses of histological features and immunological marker expression profiles of the lesion. At primary diagnosis, loco-regional metastases are already present in ∼30% of patients. Excision of the tumour is the first-line therapy; if not feasible, radiotherapy can often effectively control the disease. Chemotherapy was the only alternative in advanced-stage or refractory MCC until several clinical trials demonstrated the efficacy of immune-checkpoint inhibitors.
CD200 Expression in Neuroendocrine Neoplasms.
Love JE, Thompson K, Kilgore MR, Westerhoff M, Murphy CE, Papanicolau-Sengos A, McCormick KA, Shankaran V, Vandeven N, Miller F, Blom A, Nghiem PT, Kussick SJ.
Am J Clin Pathol. 2017 Sep 1;148(3):236-242.
PMID: 28821198
Abstract and Highlights
- OBJECTIVES: CD200 expression has been well studied in hematopoietic malignancies; however, CD200 expression has not been well-characterized in neuroendocrine neoplasms. We examined CD200 expression in 391 neuroendocrine neoplasms from various anatomic sites.
- METHODS: Tissue blocks containing pulmonary small cell carcinoma, pulmonary carcinoid, large cell neuroendocrine carcinoma, pancreatic neuroendocrine tumor, gastrointestinal carcinoid, and Merkel cell carcinoma were evaluated for CD200 expression by immunohistochemistry. A set of nonneuroendocrine carcinomas was stained for comparison.
- RESULTS: CD200 was expressed in 87% of the neuroendocrine neoplasms studied, including 60 of 72 (83%) pulmonary small cell carcinomas, 15 of 22 (68%) pulmonary carcinoids, three of four (75%) pulmonary large cell neuroendocrine carcinomas, 125 of 146 (86%) Merkel cell carcinomas, 79 of 83 (95%) gastrointestinal luminal carcinoids, and 56 of 60 (93%) pancreatic neuroendocrine tumors. Thirty-two of 157 (20%) nonneuroendocrine carcinomas expressed CD200. In gastrointestinal carcinoid and pancreatic neuroendocrine neoplasms, CD200 negativity correlated with higher grade.
- CONCLUSIONS: CD200 is a relatively sensitive marker of neuroendocrine neoplasms and represents a potential therapeutic target in these difficult-to-treat malignancies.
Immune evasion mechanisms and immune checkpoint inhibition in advanced merkel cell carcinoma.
Schadendorf D, Nghiem P, Bhatia S, Hauschild A, Saiag P, Mahnke L, Hariharan S, Kaufman HL.
Oncoimmunology. 2017 Aug 31;6(10):e1338237.
PMID: 29123950
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a rare skin cancer caused by Merkel cell polyomavirus (MCPyV) infection and/or ultraviolet radiation-induced somatic mutations. The presence of tumor-infiltrating lymphocytes is evidence that an active immune response to MCPyV and tumor-associated neoantigens occurs in some patients. However, inhibitory immune molecules, including programmed death-1 (PD-1) and programmed death-ligand 1 (PD-L1), within the MCC tumor microenvironment aid in tumor evasion of T-cell-mediated clearance. Unlike chemotherapy, treatment with anti-PD-L1 (avelumab) or anti-PD-1 (pembrolizumab) antibodies leads to durable responses in MCC, in both virus-positive and virus-negative tumors. As many tumors are established through the evasion of infiltrating immune-cell clearance, the lessons learned in MCC may be broadly relevant to many cancers.
Systematic literature review of efficacy, safety and tolerability outcomes of chemotherapy regimens in patients with metastatic Merkel cell carcinoma.
Nghiem P, Kaufman HL, Bharmal M, Mahnke L, Phatak H, Becker JC.
Future Oncol. 2017 Jun;13(14):1263-1279.
PMID: 28350180
Abstract and Highlights
- AIM: Merkel cell carcinoma (MCC) is a rare neuroendocrine, cutaneous malignancy with poor prognosis once metastasized. The aim of this study was to conduct a systematic literature review to assess clinical outcomes associated with chemotherapy regimens in metastatic MCC.
- MATERIALS & METHODS: Embase®, MEDLINE®, MEDLINE®-In-Process and CENTRAL were searched for studies published in January 2016.
- RESULTS & CONCLUSION: Overall, the literature on chemotherapy in patients with metastatic MCC is sparse, with most studies being case series/reports. Across all studies, response rates ranged from 20 to 61%, with higher response rates in first-line setting (53-61%) versus second-line setting (23-45%). Among responders, duration of response was short (≤8 months) in both first- and second-line settings. There is a need for novel agents that can induce durable responses in metastatic MCC.
Epigenetic priming restores the HLA class-I antigen processing machinery expression in Merkel cell carcinoma.
Ritter C, Fan K, Paschen A, Reker S, Ferrone S, Nghiem P, Ugurel S, Schrama D, Becker JC.
Sci Rep. 2017 May 23;7(1):2290.
PMID: 28536458
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a rare and aggressive, yet highly immunogenic skin cancer. The latter is due to its viral or UV-associated carcinogenesis. For tumor progression MCC has to escape the host’s immuno-surveillance, e.g. by loss of HLA class-I expression. Indeed, a reduced HLA class-I expression was observed in MCC tumor tissues and MCC cell lines. This reduced HLA class-I surface expression is caused by an impaired expression of key components of the antigen processing machinery (APM), including LMP2 and LMP7 as well as TAP1 and TAP2. Notably, experimental provisions of HLA class-I binding peptides restored HLA class-I surface expression on MCC cells. Silencing of the HLA class-I APM is due to histone deacetylation as inhibition of histone deacetylases (HDACs) not only induced acetylation of histones in the respective promoter regions but also re-expression of APM components. Thus, HDAC inhibition restored HLA class-I surface expression in vitro and in a mouse xenotransplantation model. In contrast to re-induction of HLA class-I by interferons, HDAC inhibitors did not interfere with the expression of immuno-dominant viral proteins. In summary, restoration of HLA class-I expression on MCC cells by epigenetic priming is an attractive approach to enhance therapies boosting adaptive immune responses.
Viral oncoprotein antibodies as a marker for recurrence of Merkel cell carcinoma: A prospective validation study.
Paulson KG, Lewis CW, Redman MW, Simonson WT, Lisberg A, Ritter D, Morishima C, Hutchinson K, Mudgistratova L, Blom A, Iyer J, Moshiri AS, Tarabadkar ES, Carter JJ, Bhatia S, Kawasumi M, Galloway DA, Wener MH, Nghiem P.
Cancer. 2017 Apr 15;123(8):1464-1474.
PMID: 27925665
Abstract and Highlights
- BACKGROUND: Merkel cell carcinoma (MCC) is an aggressive skin cancer with a recurrence rate of >40%. Of the 2000 MCC cases per year in the United States, most are caused by the Merkel cell polyomavirus (MCPyV). Antibodies to MCPyV oncoprotein (T-antigens) have been correlated with MCC tumor burden. The present study assesses the clinical utility of MCPyV-oncoprotein antibody titers for MCC prognostication and surveillance.
- METHODS: MCPyV-oncoprotein antibody detection was optimized in a clinical laboratory. A cohort of 219 patients with newly diagnosed MCC were followed prospectively (median follow-up, 1.9 years). Among the seropositive patients, antibody titer and disease status were serially tracked.
- RESULTS: Antibodies to MCPyV oncoproteins were rare among healthy individuals (1%) but were present in most patients with MCC (114 of 219 patients [52%]; P < .01). Seropositivity at diagnosis independently predicted decreased recurrence risk (hazard ratio, 0.58; P = .04) in multivariate analyses adjusted for age, sex, stage, and immunosuppression. After initial treatment, seropositive patients whose disease did not recur had rapidly falling titers that became negative by a median of 8.4 months. Among seropositive patients who underwent serial evaluation (71 patients; 282 time points), an increasing oncoprotein titer had a positive predictive value of 66% for clinically evident recurrence, whereas a decreasing titer had a negative predictive value of 97%.
- CONCLUSIONS: Determination of oncoprotein antibody titer assists in the clinical management of patients with newly diagnosed MCC by stratifying them into a higher risk seronegative cohort, in which radiologic imaging may play a more prominent role, and into a lower risk seropositive cohort, in which disease status can be tracked in part by oncoprotein antibody titer. Cancer 2017;123:1464-1474. © 2016 American Cancer Society.
DGCR8 Mediates Repair of UV-Induced DNA Damage Independently of RNA Processing.
Calses PC, Dhillon KK, Tucker N, Chi Y, Huang J, Kawasumi M, Nghiem P, Wang Y, Clurman BE, Jacquemont C, Gafken PR, Sugasawa K, Saijo M, Taniguchi T.
Cell Rep. 2017 Apr 4;19(1):162-174.
PMID: 28380355
Abstract and Highlights
- Ultraviolet (UV) radiation is a carcinogen that generates DNA lesions. Here, we demonstrate an unexpected role for DGCR8, an RNA binding protein that canonically functions with Drosha to mediate microRNA processing, in the repair of UV-induced DNA lesions. Treatment with UV induced phosphorylation on serine 153 (S153) of DGCR8 in both human and murine cells. S153 phosphorylation was critical for cellular resistance to UV, the removal of UV-induced DNA lesions, and the recovery of RNA synthesis after UV exposure but not for microRNA expression. The RNA-binding and Drosha-binding activities of DGCR8 were not critical for UV resistance. DGCR8 depletion was epistatic to defects in XPA, CSA, and CSB for UV sensitivity. DGCR8 physically interacted with CSB and RNA polymerase II. JNKs were involved in the UV-induced S153 phosphorylation. These findings suggest that UV-induced S153 phosphorylation mediates transcription-coupled nucleotide excision repair of UV-induced DNA lesions in a manner independent of microRNA processing.
Polyomavirus-Negative Merkel Cell Carcinoma: A More Aggressive Subtype Based on Analysis of 282 Cases Using Multimodal Tumor Virus Detection.
Moshiri AS, Doumani R, Yelistratova L, Blom A, Lachance K, Shinohara MM, Delaney M, Chang O, McArdle S, Thomas H, Asgari MM, Huang ML, Schwartz SM, Nghiem P.
J Invest Dermatol. 2017 Apr;137(4):819-827.
PMID: 27815175
View Abstract and Highlights
- Previous studies have reached conflicting conclusions regarding the proportion of Merkel cell carcinomas (MCCs) that contain the Merkel cell polyomavirus (MCPyV) and the clinical significance of tumor viral status. To address these controversies, we detected MCPyV large T antigen using immunohistochemistry with two distinct antibodies and MCPyV DNA using quantitative PCR. Tumors were called MCPyV-positive if two or more of these three assays indicated presence of this virus. A total of 53 of 282 (19%) MCC tumors in this cohort were virus-negative using this multimodal system. Immunohistochemistry with the CM2B4 antibody had the best overall performance (sensitivity = 0.882, specificity = 0.943) compared with the multimodal classification. Multivariate analysis including age, sex, and immunosuppression showed that, relative to MCC patients with virus-positive tumors, virus-negative MCC patients had significantly increased risk of disease progression (hazard ratio = 1.77, 95% confidence interval = 1.20-2.62) and death from MCC (hazard ratio = 1.85, 95% confidence interval = 1.19-2.89). We confirm that approximately 20% of MCCs are not driven by MCPyV and that such virus-negative MCCs, which can be quite reliably identified by immunohistochemistry using the CM2B4 antibody alone, represent a more aggressive subtype that warrants closer clinical follow-up.
Biomedical Research as a Team Sport.
Nghiem P.
J Invest Dermatol. 2017 Apr;137(4):783-786.
PMID: 28340678
Factors influencing radiation treatment recommendations in early-stage Merkel cell carcinoma: a survey of US-based radiation oncologists.
Tseng YD, Apisarnthanarax S, Liao JJ, Bhatia S, Nghiem PT, Parvathaneni U.
Expert Rev Anticancer Ther. 2017 Mar;17(3):281-287.
PMID: 28103445
Abstract and Highlights
- BACKGROUND: It is unclear which subgroups of Merkel cell carcinoma (MCC) patients benefit the most from radiation. We surveyed radiation oncologists (RO) that regularly see and treat MCC to understand how they approach the treatment of early-stage MCC.
- METHODS: A web-based survey was emailed to 63 ROs, who were identified through publications, guideline panel membership, and/or affiliation with institutions of high MCC volume. ROs provided treatment recommendations for two hypothetical case scenarios of early stage MCC.
- RESULTS: Among 28 respondents (45%), 26 regularly saw and treated MCC patients for a median 7 years (range, 0-30). While all ROs recommended adjuvant radiation for a stage II upper extremity MCC, only 48% recommended adjuvant radiation for stage I head and neck MCC.
- CONCLUSION: Among US-based MCC RO ‘specialists,’ there is equipoise on the role of radiotherapy for stage I MCC. Ideally, prospective studies are needed to identify which patients may benefit from radiation.
Tumor-Infiltrating Merkel Cell Polyomavirus-Specific T Cells Are Diverse and Associated with Improved Patient Survival.
Miller NJ, Church CD, Dong L, Crispin D, Fitzgibbon MP, Lachance K, Jing L, Shinohara M, Gavvovidis I, Willimsky G, McIntosh M, Blankenstein T, Koelle DM, Nghiem P.
Cancer Immunol Res. 2017 Feb;5(2):137-147.
PMID: 28093446
Abstract and Highlights
- Tumor-infiltrating CD8+ T cells are associated with improved survival of patients with Merkel cell carcinoma (MCC), an aggressive skin cancer causally linked to Merkel cell polyomavirus (MCPyV). However, CD8+ T-cell infiltration is robust in only 4% to 18% of MCC tumors. We characterized the T-cell receptor (TCR) repertoire restricted to one prominent epitope of MCPyV (KLLEIAPNC, “KLL”) and assessed whether TCR diversity, tumor infiltration, or T-cell avidity correlated with clinical outcome. HLA-A*02:01/KLL tetramer+ CD8+ T cells from MCC patient peripheral blood mononuclear cells (PBMC) and tumor-infiltrating lymphocytes (TIL) were isolated via flow cytometry. TCRβ (TRB) sequencing was performed on tetramer+ cells from PBMCs or TILs (n = 14) and matched tumors (n = 12). Functional avidity of T-cell clones was determined by IFNγ production. We identified KLL tetramer+ T cells in 14% of PBMC and 21% of TIL from MCC patients. TRB repertoires were strikingly diverse (397 unique TRBs were identified from 12 patients) and mostly private (only one TCRb clonotype shared between two patients). An increased fraction of KLL-specific TIL (>1.9%) was associated with significantly increased MCC-specific survival P = 0.0009). T-cell cloning from four patients identified 42 distinct KLL-specific TCRa/b pairs. T-cell clones from patients with improved MCC-specific outcomes were more avid (P < 0.05) and recognized an HLA-appropriate MCC cell line. T cells specific for a single MCPyV epitope display marked TCR diversity within and between patients. Intratumoral infiltration by MCPyV-specific T cells was associated with significantly improved MCC-specific survival, suggesting that augmenting the number or avidity of virus-specific T cells may have therapeutic benefit. Cancer Immunol Res; 5(2); 137-47.
2016
Postoperative radiation therapy is associated with a reduced risk of local recurrence among low risk Merkel cell carcinomas of the head and neck.
Takagishi SR, Marx TE, Lewis C, Tarabadker ES, Juhlin ID, Blom A, Iyer JG, Liao JJ, Tseng YD, Fu T, Nghiem P, Parvathaneni U.
Adv Radiat Oncol. 2016 Oct 20;1(4):244-251.
PMID: 28740894
Abstract and Highlights
- PURPOSE: Merkel cell carcinoma (MCC) is a rare and often aggressive skin cancer. Typically, surgery is the primary treatment. Postoperative radiation therapy (PORT) is often recommended to improve local control. It is unclear whether PORT is indicated in patients with favorable Stage IA head and neck (HN) MCC.
- METHODS AND MATERIALS: We conducted a retrospective analysis of 46 low-risk HN MCC cases treated between 2006 and 2015. Inclusion criteria were defined as a primary tumor size of ≤ 2 cm, negative pathological margins, negative sentinel lymph node biopsy, and no immunosuppression. Local recurrence (LR) was defined as tumor recurrence within 2 cm of the primary surgical bed and estimated with the Kaplan-Meier method.
- RESULTS: Omission of PORT was offered to all 46 patients, of which 23 patients received PORT and 23 did not. No patient received adjuvant chemotherapy. There were no significant differences in surgical margins, tumor size, depth, lympho-vascular invasion status, or demographics between the two patient groups. Median follow-up for all patients was 3.7 years. Six of the 23 patients who did not receive PORT developed an LR. Compared to the group that received PORT, there was a significantly higher risk of LR in the group treated without PORT (26% vs. 0%, P = .02). Median time to LR was 11 months. All local failures were effectively salvaged. There was no difference in MCC-specific and overall survival between the 2 groups.
- CONCLUSIONS: For patients with HN MCC, omission of PORT was associated with a significantly higher risk of local recurrence even among those patients with the lowest-risk tumors (i.e., Stage IA without immune suppression). Thus, it is important to weigh the benefits of PORT against the side effect profile on a case-specific basis for each patient.
Avelumab in patients with chemotherapy-refractory metastatic Merkel cell carcinoma: a multicentre, single-group, open-label, phase 2 trial.
Kaufman HL, Russell J, Hamid O, Bhatia S, Terheyden P, D'Angelo SP, Shih KC, Lebbé C, Linette GP, Milella M, Brownell I, Lewis KD, Lorch JH, Chin K, Mahnke L, von Heydebreck A, Cuillerot JM, Nghiem P.
Lancet Oncol. 2016 Oct;17(10):1374-1385.
PMID: 27592805
Abstract and Highlights
- BACKGROUND: Merkel cell carcinoma is a rare, aggressive skin cancer with poor prognosis in patients with advanced disease. Current standard care uses various cytotoxic chemotherapy regimens, but responses are seldom durable. Tumour oncogenesis is linked to Merkel cell polyomavirus integration and ultraviolet-radiation-induced mutations, providing rationale for treatment with immunotherapy antibodies that target the PD-L1/PD-1 pathway. We assessed treatment with avelumab, an anti-PD-L1 monoclonal antibody, in patients with stage IV Merkel cell carcinoma that had progressed after cytotoxic chemotherapy.
- METHODS: In this multicentre, international, prospective, single-group, open-label, phase 2 trial, patients with stage IV chemotherapy-refractory, histologically confirmed Merkel cell carcinoma (aged ≥18 years) were enrolled from 35 cancer treatment centres and academic hospitals in North America, Europe, Australia, and Asia. Key eligibility criteria were an ECOG performance status of 0 or 1, measurable disease by Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1, adequate haematological, hepatic, and renal function, and immune-competent status (patients with HIV, immunosuppression, haematological malignancies, and previous organ transplantation were excluded). Patient selection was not based on PD-L1 expression or Merkel cell polyomavirus status. Collection of biopsy material or use of archival tissue for these assessments was mandatory. Avelumab was given intravenously at a dose of 10 mg/kg every 2 weeks. The primary endpoint was confirmed objective response (complete response or partial response) assessed according to RECIST version 1.1 by an independent review committee. Safety and clinical activity were assessed in all patients who received at least one dose of study drug (the modified intention-to-treat population). This trial is registered with ClinicalTrials.gov as NCT02155647.
- FINDINGS: Between July 25, 2014, and Sept 3, 2015, 88 patients were enrolled and received at least one dose of avelumab. Patients were followed up for a median of 10·4 months (IQR 8·6-13·1). The proportion of patients who achieved an objective response was 28 (31·8% [95·9% CI 21·9-43·1]) of 88 patients, including eight complete responses and 20 partial responses. Responses were ongoing in 23 (82%) of 28 patients at the time of analysis. Five grade 3 treatment-related adverse events occurred in four (5%) patients: lymphopenia in two patients, blood creatine phosphokinase increase in one patient, aminotransferase increase in one patient, and blood cholesterol increase in one patient; there were no treatment-related grade 4 adverse events or treatment-related deaths. Serious treatment-related adverse events were reported in five patients (6%): enterocolitis, infusion-related reaction, aminotransferases increased, chondrocalcinosis, synovitis, and interstitial nephritis (n=1 each).
- INTERPRETATION: Avelumab was associated with durable responses, most of which are still ongoing, and was well tolerated; hence, avelumab represents a new therapeutic option for advanced Merkel cell carcinoma.
- FUNDING: Merck KGaA, Darmstadt, Germany.
Analysis of Prognostic Factors from 9387 Merkel Cell Carcinoma Cases Forms the Basis for the New 8th Edition AJCC Staging System.
Harms KL, Healy MA, Nghiem P, Sober AJ, Johnson TM, Bichakjian CK, Wong SL.
Ann Surg Oncol. 2016 Oct;23(11):3564-3571.
PMID: 27198511
Abstract and Highlights
- BACKGROUND: The first consensus Merkel cell carcinoma (MCC) staging system was published in 2010. New information on the clinical course prompts review of MCC staging.
- METHODSA total of 9387 MCC cases from the National Cancer Data Base Participant User File with follow-up and staging data (1998-2012) were analyzed. Prognostic differences based on clinical and pathological staging were evaluated. Survival estimates were compared by disease extent.
- RESULTS: Sixty-five percent of cases presented with local disease, whereas 26 and 8 % presented with nodal and distant disease. Disease extent at presentation was predictive of 5-year overall survival (OS) with estimates of 51, 35, and 14 % for local, nodal, and distant disease. Tumor burden at the regional nodal basin was predictive of 5-year OS with estimates of 40 and 27 % for clinically occult and clinically detected nodal disease. For local disease, we confirm improved prognosis when the regional nodal basin was negative by pathological compared with clinical staging. We identified 336 cases with clinically detected nodal disease and unknown primary tumor and showed improved prognosis over cases presenting with concurrent primary tumor (OS estimates of 42 vs. 27 %).
- CONCLUSIONS: Analysis of a national dataset of MCC cases validates the predictive value of disease extent at presentation. Separation of clinical and pathological stage groups and regrouping of unknown primary tumors are supported by the analysis. The revised staging system provides more accurate prognostication and has been formally accepted by the AJCC staging committee for inclusion in the 8th edition.
Paraneoplastic syndromes (PNS) associated with Merkel cell carcinoma (MCC): A case series of 8 patients highlighting different clinical manifestations.
Iyer JG, Parvathaneni K, Bhatia S, Tarabadkar ES, Blom A, Doumani R, McKenzie J, Asgari MM, Nghiem P.
J Am Acad Dermatol. 2016 Sep;75(3):541-547.
PMID: 27177440
Abstract and Highlights
- BACKGROUND: Paraneoplastic syndromes (PNS) are commonly associated with neuroendocrine cancers, such as small cell lung cancer.
- OBJECTIVES: We examined the association of PNS in Merkel cell carcinoma (MCC), a rare neuroendocrine skin cancer.
- METHODS: We identified PNS associated with MCC based on chart review of a Seattle-based repository and examined the incidence of MCC-associated hyponatremia in an independent cohort within Kaiser Permanente Northern California.
- RESULTS: Eight PNS cases were identified from the Seattle repository. Three distinct PNS types were observed: cerebellar degeneration (1 case), Lambert-Eaton myasthenic syndrome (2 cases), and malignancy-associated hyponatremia (5 cases). Moreover, the incidence of severe hyponatremia (serum sodium <125 mmol/L) coincident with MCC was identified among 4.3% (9 of 211) patients with MCC in the Kaiser Permanente Northern California cohort.
- LIMITATIONS: We did not have access to complete medical records on all patients so it was not possible to determine the prevalence of PNS in MCC.
- CONCLUSIONS: MCC can be associated with PNS similar to those found in other neuroendocrine cancers. Clinicians should be aware of these presentations as PNS often precede the identification of the underlying malignancy and usually resolve with appropriate treatment of the cancer.
Response rates and durability of chemotherapy among 62 patients with metastatic Merkel cell carcinoma.
Iyer JG, Blom A, Doumani R, Lewis C, Tarabadkar ES, Anderson A, Ma C, Bestick A, Parvathaneni U, Bhatia S, Nghiem P.
Cancer Med. 2016 Sep;5(9):2294-301.
PMID: 27431483
Abstract and Highlights
- Cytotoxic chemotherapy is commonly used to treat advanced Merkel cell carcinoma (MCC). However, its efficacy in distant metastatic MCC patients is unclear, in part because most prior reports aggregated these patients with those receiving adjuvant chemotherapy and combined chemoradiation for whom prognosis and outcomes may differ. In this retrospective study, we analyzed detailed records from 62 patients with distant metastatic MCC treated with cytotoxic chemotherapy. Efficacy outcomes including response rate (RR), durability of response (DOR), progression-free survival (PFS), and overall survival (OS) were evaluated. In this cohort, platinum plus etoposide was the most commonly used first-line regimen (69%). RR to first-line chemotherapy was 55% (34/62) with complete responses (CR) in 13% (8/62) and partial responses (PR) in 42% (26/62) while 6% (4/62) had stable disease and 39% (24/62) had progressive disease. Median PFS was 94 days and median OS was 9.5 months from start of chemotherapy. Among responding patients (n = 34), median PFS was 168 days and median DOR was 85 days. Among 30 of the 62 patients who received second-line chemotherapy, RR was 23% (7/30; 1 CR, 6 PR), median PFS was 61 days, and median DOR was 101 days. In summary, first-line chemotherapy is associated with a high RR in metastatic MCC, but responses are typically not durable, and the median PFS is only 3 months. These results suggest rapid emergence of chemoresistance in MCC tumors, and may serve as a useful comparator for immunotherapies currently being explored for metastatic MCC.
Merkel Cell Carcinoma: An Unusually Immunogenic Cancer Proves Ripe for Immune Therapy.
Vandeven N, Nghiem P.
J Oncol Pract. 2016 Jul;12(7):649-50.
PMID: 27407162
Rationale for immune-based therapies in Merkel polyomavirus-positive and -negative Merkel cell carcinomas.
Vandeven N, Nghiem P.
Immunotherapy. 2016 Jul;8(8):907-21.
PMID: 27381685
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a rare but often deadly skin cancer that is typically caused by the Merkel cell polyomavirus (MCPyV). Polyomavirus T-antigen oncoproteins are persistently expressed in virus-positive MCCs (˜80% of cases), while remarkably high numbers of tumor-associated neoantigens are detected in virus-negative MCCs, suggesting that both MCC subsets may be immunogenic. Here we review mechanisms by which these immunogenic tumors evade multiple levels of host immunity. Additionally, we summarize the exciting potential of diverse immune-based approaches to treat MCC. In particular, agents blocking the PD-1 axis have yielded strikingly high response rates in MCC as compared with other solid tumors, highlighting the potential for immune-mediated treatment of this disease.
PD-1 Blockade with Pembrolizumab in Advanced Merkel-Cell Carcinoma.
Nghiem PT, Bhatia S, Lipson EJ, Kudchadkar RR, Miller NJ, Annamalai L, Berry S, Chartash EK, Daud A, Fling SP, Friedlander PA, Kluger HM, Kohrt HE, Lundgren L, Margolin K, Mitchell A, Olencki T, Pardoll DM, Reddy SA, Shantha EM, Sharfman WH, Sharon E, Shemanski LR, Shinohara MM, Sunshine JC, Taube JM, Thompson JA, Townson SM, Yearley JH, Topalian SL, Cheever MA.
N Engl J Med. 2016 Jun 30;374(26):2542-52.
PMID: 27093365
Abstract and Highlights
- BACKGROUND: Merkel-cell carcinoma is an aggressive skin cancer that is linked to exposure to ultraviolet light and the Merkel-cell polyomavirus (MCPyV). Advanced Merkel-cell carcinoma often responds to chemotherapy, but responses are transient. Blocking the programmed death 1 (PD-1) immune inhibitory pathway is of interest, because these tumors often express PD-L1, and MCPyV-specific T cells express PD-1.
- METHODS: In this multicenter, phase 2, noncontrolled study, we assigned adults with advanced Merkel-cell carcinoma who had received no previous systemic therapy to receive pembrolizumab (anti-PD-1) at a dose of 2 mg per kilogram of body weight every 3 weeks. The primary end point was the objective response rate according to Response Evaluation Criteria in Solid Tumors, version 1.1. Efficacy was correlated with tumor viral status, as assessed by serologic and immunohistochemical testing.
- RESULTS: A total of 26 patients received at least one dose of pembrolizumab. The objective response rate among the 25 patients with at least one evaluation during treatment was 56% (95% confidence interval [CI], 35 to 76); 4 patients had a complete response, and 10 had a partial response. With a median follow-up of 33 weeks (range, 7 to 53), relapses occurred in 2 of the 14 patients who had had a response (14%). The response duration ranged from at least 2.2 months to at least 9.7 months. The rate of progression-free survival at 6 months was 67% (95% CI, 49 to 86). A total of 17 of the 26 patients (65%) had virus-positive tumors. The response rate was 62% among patients with MCPyV-positive tumors (10 of 16 patients) and 44% among those with virus-negative tumors (4 of 9 patients). Drug-related grade 3 or 4 adverse events occurred in 15% of the patients.
- CONCLUSIONS: In this study, first-line therapy with pembrolizumab in patients with advanced Merkel-cell carcinoma was associated with an objective response rate of 56%. Responses were observed in patients with virus-positive tumors and those with virus-negative tumors. (Funded by the National Cancer Institute and Merck; ClinicalTrials.gov number, NCT02267603.).
Adjuvant Radiation Therapy and Chemotherapy in Merkel Cell Carcinoma: Survival Analyses of 6908 Cases From the National Cancer Data Base.
Bhatia S, Storer BE, Iyer JG, Moshiri A, Parvathaneni U, Byrd D, Sober AJ, Sondak VK, Gershenwald JE, Nghiem P.
J Natl Cancer Inst. 2016 May 31;108(9).
PMID: 27245173
Abstract and Highlights
- BACKGROUND: Merkel cell carcinoma (MCC) has a high risk of recurrence after initial surgical therapy. Adjuvant radiation therapy (RT) and chemotherapy may be used to reduce the risk of locoregional and systemic recurrence, respectively, but there are conflicting data regarding their impact on survival. We performed a retrospective analysis of MCC cases from the National Cancer Data Base (NCDB) to assess whether adjuvant therapy was associated with differences in survival.
- METHODS: Six thousand nine hundred and eight MCC patients with staging, treatment, and survival data were included. Multivariable analyses were conducted for overall survival (OS) with various treatment modalities while adjusting for prognostic variables including age, sex, comorbidities (Charlson/Deyo score), margin status, primary tumor site and size, and lymph node status. All statistical tests were two-sided.
- RESULTS: For localized MCC (stage I: n = 3369, stage II: n = 1474 ), surgery plus adjuvant RT was associated with statistically significantly better OS than with surgery alone in multivariable analyses (stage I: hazard ratio [HR] = 0.71, 95% confidence interval [CI] = 0.64 to 0.80, P < .001; stage II: HR = 0.77, 95% CI = 0.66 to 0.89, P < .001). In patients with regional nodal metastases (stage III: n = 2065 ), neither adjuvant RT nor chemotherapy was associated with statistically significantly improved or worsened OS.
- CONCLUSIONS: In this study of the largest MCC cohort reported to date, adjuvant RT was associated with improved OS in stages I-II MCC. Neither adjuvant RT nor chemotherapy was associated with improved OS in stage III MCC. These results, with the limitations of retrospective analyses, are consistent with earlier studies suggesting benefit with adjuvant RT but do not support the routine use of adjuvant chemotherapy in MCC.
Basal Cell Skin Cancer, Version 1.2016, NCCN Clinical Practice Guidelines in Oncology.
Bichakjian CK, Olencki T, Aasi SZ, Alam M, Andersen JS, Berg D, Bowen GM, Cheney RT, Daniels GA, Glass LF, Grekin RC, Grossman K, Higgins SA, Ho AL, Lewis KD, Lydiatt DD, Nehal KS, Nghiem P, Olsen EA, Schmults CD, Sekulic A, Shaha AR, Thorstad WL, Tuli M, Urist MM, Wang TS, Wong SL, Zic JA, Hoffmann KG, Engh A.
J Natl Compr Canc Netw. 2016 May;14(5):574-97.
PMID: 27160235
Abstracts and Highlights
- Basal cell carcinoma (BCC) of the skin is the most common cancer, with a higher incidence than all other malignancies combined. Although it is rare to metastasize, patients with multiple or frequently recurring BCC can suffer substantial comorbidity and be difficult to manage. Assessment of risk is a key element of management needed to inform treatment selection. The overall management of BCC primarily consists of surgical approaches, with radiation therapy as an alternate or adjuvant option. Many superficial therapies for BCC have been explored and continue to be developed, including topicals, cryosurgery, and photodynamic therapy. Two hedgehog pathway inhibitors were recently approved by the FDA for systemic treatment of advanced and metastatic BCC, and others are in development. The NCCN Guidelines for Basal Cell Skin Cancer, published in full herein, include recommendations for selecting among the various surgical approaches based on patient-, lesion-, and disease-specific factors, as well as guidance on when to use radiation therapy, superficial therapies, and hedgehog pathway inhibitors.
Reversal of epigenetic silencing of MHC class I chain-related protein A and B improves immune recognition of Merkel cell carcinoma.
Ritter C, Fan K, Paulson KG, Nghiem P, Schrama D, Becker JC.
Sci Rep. 2016 Feb 23;6:21678.
PMID: 26902929
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a virally associated cancer characterized by its aggressive behavior and strong immunogenicity. Both viral infection and malignant transformation induce expression of MHC class I chain-related protein (MIC) A and B, which signal stress to cells of the immune system via Natural Killer group 2D (NKG2D) resulting in elimination of target cells. However, despite transformation and the continued presence of virally-encoded proteins, MICs are only expressed in a minority of MCC tumors in situ and are completely absent on MCC cell lines in vitro. This lack of MIC expression was due to epigenetic silencing via MIC promoter hypo-acetylation; indeed, MIC expression was re-induced by pharmacological inhibition of histone deacetylases (HDACs) both in vitro and in vivo. This re-induction of MICs rendered MCC cells more sensitive to immune-mediated lysis. Thus, epigenetic silencing of MICs is an important immune escape mechanism of MCCs.
Mutational landscape of MCPyV-positive and MCPyV-negative Merkel cell carcinomas with implications for immunotherapy.
Goh G, Walradt T, Markarov V, Blom A, Riaz N, Doumani R, Stafstrom K, Moshiri A, Yelistratova L, Levinsohn J, Chan TA, Nghiem P, Lifton RP, Choi J.
Oncotarget. 2016 Jan 19;7(3):3403-15.
PMID: 26655088
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a rare but highly aggressive cutaneous neuroendocrine carcinoma, associated with the Merkel cell polyomavirus (MCPyV) in 80% of cases. To define the genetic basis of MCCs, we performed exome sequencing of 49 MCCs. We show that MCPyV-negative MCCs have a high mutation burden (median of 1121 somatic single nucleotide variants (SSNVs) per-exome with frequent mutations in RB1 and TP53 and additional damaging mutations in genes in the chromatin modification (ASXL1, MLL2, and MLL3), JNK (MAP3K1 and TRAF7), and DNA-damage pathways (ATM, MSH2, and BRCA1). In contrast, MCPyV-positive MCCs harbor few SSNVs (median of 12.5 SSNVs/tumor) with none in the genes listed above. In both subgroups, there are rare cancer-promoting mutations predicted to activate the PI3K pathway (HRAS, KRAS, PIK3CA, PTEN, and TSC1) and to inactivate the Notch pathway (Notch1 and Notch2). TP53 mutations appear to be clinically relevant in virus-negative MCCs as 37% of these tumors harbor potentially targetable gain-of-function mutations in TP53 at p.R248 and p.P278. Moreover, TP53 mutational status predicts death in early stage MCC (5-year survival in TP53 mutant vs wild-type stage I and II MCCs is 20% vs. 92%, respectively; P = 0.0036). Lastly, we identified the tumor neoantigens in MCPyV-negative and MCPyV-positive MCCs. We found that virus-negative MCCs harbor more tumor neoantigens than melanomas or non-small cell lung cancers (median of 173, 65, and 111 neoantigens/sample, respectively), two cancers for which immune checkpoint blockade can produce durable clinical responses. Collectively, these data support the use of immunotherapies for virus-negative MCCs.
2015
Why Do Airline Pilots and Flight Crews Have an Increased Incidence of Melanoma?
Shantha E, Lewis C, Nghiem P.
JAMA Oncol. 2015 Sep;1(6):829-30.
PMID: 26181192
Single fraction radiation therapy in patients with metastatic Merkel cell carcinoma.
Iyer JG, Parvathaneni U, Gooley T, Miller NJ, Markowitz E, Blom A, Lewis CW, Doumani RF, Parvathaneni K, Anderson A, Bestick A, Liao J, Kane G, Bhaftia S, Paulson K, Nghiem P.
Cancer Med. 2015 Aug;4(8):1161-70.
PMID: 25908228
Abstract and Highlights
- Merkel cell carcinoma (MCC) is an aggressive, polyomavirus-associated cancer with limited therapeutic options for metastatic disease. Cytotoxic chemotherapy is associated with high response rates, but responses are seldom durable and toxicity is considerable. Here, we report our experience with palliative single-fraction radiotherapy (SFRT) in patients with metastatic MCC. We conducted retrospective analyses of safety and efficacy outcomes in patients that received SFRT (8 Gy) to MCC metastases between 2010 and 2013. Twenty-six patients were treated with SFRT to 93 MCC tumors located in diverse sites that included skin, lymph nodes, and visceral organs. Objective responses were observed in 94% of the measurable irradiated tumors (86/92). Complete responses were observed in 45% of tumors (including bulky tumors up to 16 cm). “In field” lesion control was durable with no progression in 77% (69/89) of treated tumors during median follow-up of 277 days among 16 living patients. Clinically significant toxicity was seen in only two patients who had transient side effects. An exploratory analysis suggested a higher rate of in-field progression in patients with an immunosuppressive comorbidity or prior recent chemotherapy versus those without (30% and 9%, respectively; P = 0.03). Use of SFRT in palliating MCC patients was associated with an excellent in field control rate and durable responses at treated sites, and with minimal toxicity. SFRT may represent a convenient and appealing alternative to systemic chemotherapy for palliation, for which most patients with oligometastatic MCC are eligible. SFRT may also synergize with emerging systemic immune stimulants by lowering tumor burden and enhancing presentation of viral/tumor antigens.
Merkel Cell Carcinoma: Intersection of Immune Dysfunction, Infection, and Malignant Progression.
Nghiem P.
J Investig Dermatol Symp Proc. 2015 Jul;17(1):36.
PMID: 26067317
How does the Merkel polyomavirus transform cells? Many answers, many questions, and a new mouse model.
Church C., Nghiem P.
J Invest Dermatol. 2015 May;135(5):1221-1224.
PMID: 25882464
Abstract and Highlights
- The Merkel cell polyomavirus (MCPyV), discovered in 2008, drives the development of most Merkel cell carcinomas (MCCs) through several canonical mechanisms. A glaring gap in our knowledge remains the basis by which MCPyV, among all 12 human polyomaviruses, is the only one that causes cancer in humans. Moreover, initial attempts by numerous groups have failed to reproduce MCC in mice using oncoproteins from this polyomavirus. Verhaegen et al. report MCPyV small T-antigen-expressing transgenic mice that now provide insight into in vivo transformation mechanisms.
2014
Identification of ATR-Chk1 Pathway Inhibitors That Selectively Target p53-Deficient Cells without Directly Suppressing ATR Catalytic Activity.
Kawasumi M, Bradner JE, Tolliday N, Thibodeau R, Sloan H, Brummond KM, Nghiem P.
Cancer Res. 2014 Dec 15;74(24):7534-45.
PMID: 25336189
Abstract and Highlights
- Resistance to DNA-damaging chemotherapy is a barrier to effective treatment that appears to be augmented by p53 functional deficiency in many cancers. In p53-deficient cells in which the G1-S checkpoint is compromised, cell viability after DNA damage relies upon intact intra-S and G2-M checkpoints mediated by the ATR (ataxia telangiectasia and Rad3 related) and Chk1 kinases. Thus, a logical rationale to sensitize p53-deficient cancers to DNA-damaging chemotherapy is through the use of ATP-competitive inhibitors of ATR or Chk1. To discover small molecules that may act on uncharacterized components of the ATR pathway, we performed a phenotype-based screen of 9,195 compounds for their ability to inhibit hydroxyurea-induced phosphorylation of Ser345 on Chk1, known to be a critical ATR substrate. This effort led to the identification of four small-molecule compounds, three of which were derived from known bioactive library (anthothecol, dihydrocelastryl, and erysolin) and one of which was a novel synthetic compound termed MARPIN. These compounds all inhibited ATR-selective phosphorylation and sensitized p53-deficient cancer cells to DNA-damaging agents in vitro and in vivo. Notably, these compounds did not inhibit ATR catalytic activity in vitro, unlike typical ATP-competitive inhibitors, but acted in a mechanistically distinct manner to disable ATR-Chk1 function. Our results highlight a set of novel molecular probes to further elucidate druggable mechanisms to improve cancer therapeutic responses produced by DNA-damaging drugs.
Downregulation of MHC-1 expression is prevalent but reversible in Merkel cell carcinoma.
Paulson KG, Tegeder A, Willmes C, Iyer JG, Afanasiev OK, Schrama D, Koba S, Thibodeau R, Nagase K, Simonson WT, Seo A, Koelle DM, Madeleine M, Bhatia S, Nakajima H, Sano S, Hardwick JS, Disis ML, Cleary MA, Becker JC, Nghiem P.
Cancer Immunol Res. 2014 Nov;2(11):1071-9.
PMID: 25116754
Abstract and Highlights
- Merkel cell carcinoma (MCC) is an aggressive, polyomavirus-associated skin cancer. Robust cellular immune responses are associated with excellent outcomes in patients with MCC, but these responses are typically absent. We determined the prevalence and reversibility of major histocompatibility complex class I (MHC-I) downregulation in MCC, a potentially reversible immune-evasion mechanism. Cell-surface MHC-I expression was assessed on five MCC cell lines using flow cytometry as well as immunohistochemistry on tissue microarrays representing 114 patients. Three additional patients were included who had received intralesional IFN treatment and had evaluable specimens before and after treatment. mRNA expression analysis of antigen presentation pathway genes from 35 MCC tumors was used to examine the mechanisms of downregulation. Of note, 84% of MCCs (total n = 114) showed reduced MHC-I expression as compared with surrounding tissues, and 51% had poor or undetectable MHC-I expression. Expression of MHC-I was lower in polyomavirus-positive MCCs than in polyomavirus-negative MCCs (P < 0.01). The MHC-I downregulation mechanism was multifactorial and did not depend solely on HLA gene expression. Treatment of MCC cell lines with ionizing radiation, etoposide, or IFN resulted in MHC-I upregulation, with IFNs strongly upregulating MHC-I expression in vitro, and in 3 of 3 patients treated with intralesional IFNs. MCC tumors may be amenable to immunotherapy, but downregulation of MHC-I is frequently present in these tumors, particularly those that are positive for polyomavirus. This downregulation is reversible with any of several clinically available treatments that may thus promote the effectiveness of immune-stimulating therapies for MCC.
CD8+ lymphocyte intratumoral infiltration as a stage-independent predictor of Merkel cell carcinoma survival: a population-based study.
Paulson KG, Iyer JG, Simonson WT, Blom A, Thibodeau RM, Schmidt M, Pietromonaco S, Sokil M, Warton EM, Asgari MM, Nghiem P.
Am J Clin Pathol. 2014 Oct;142(4):452-8.
PMID: 25239411
Abstract and Highlights
- OBJECTIVES: Intratumoral CD8+ lymphocytes (IT-CD8s) have shown promise as a prognostic indicator for Merkel cell carcinoma (MCC). We tested whether IT-CD8s predict survival among a population-based MCC cohort.
- METHODS: One hundred thirty-seven MCC cases that had not previously been analyzed for IT-CD8s were studied.
- RESULTS: Three-year MCC-specific survival rates were 56%, 72%, and 100% for patients with absent (n = 46), low (n = 85), and moderate or strong (n = 6) IT-CD8s, respectively. Increased IT-CD8s were associated with improved MCC-specific survival in a multivariate competing risk-regression analysis including stage, age, and sex (hazard ratio [HR] = 0.5; 95% confidence interval [CI] = 0.3-0.9). Although a similar trend was observed for overall survival, statistical significance was not reached (HR = 0.8; 95% CI = 0.6-1.0), likely because of the high rate of non-MCC deaths among older patients.
- CONCLUSIONS: This study of prospectively captured MCC cases supports the concept that cellular immuni
Milestones in the staging, classification, and biology of Merkel cell carcinoma.
Moshiri AS, Nghiem P.
J Natl Compr Canc Netw. 2014 Sep;12(9):1255-62.
PMID: 25190694
Abstract and Highlights
- Merkel cell carcinoma (MCC) is an aggressive skin cancer that is causally associated with ultraviolet light exposure and a recently discovered polyomavirus. Before 2010, MCC was staged using any of 5 unique systems in active use. In 2010, a consensus staging system for MCC was adopted worldwide and replaced these systems. This consensus system includes substages that reflect prognostic differences based on whether nodal evaluation was performed by pathologic analysis or clinical assessment alone. MCC-specific disease classification in ICD-9, to be expanded in the upcoming ICD-10, has improved the ability to track and manage this malignancy. Several biomarkers and histopathologic features have been identified that improve understanding of this cancer and may lead to future refinement of the current staging system. In 2008, the Merkel cell polyomavirus was discovered and is now thought to be a critical mechanism of transformation in at least 80% of MCCs. In patients who produce antibodies to the viral T-antigen oncoprotein, the titer increases and decreases with MCC disease burden and can be a clinically useful marker of recurrence. Diverse studies link CD8-positive T-cell function with outcomes in MCC and serve as the rational basis for ongoing trials of therapies to augment cellular immunity. This article reviews basic and translational research insights that will lead to improved staging, prognostic accuracy, and mechanism-based therapy for this often-lethal skin cancer.
Effect of host, tumor, diagnostic, and treatment variables on outcomes in a large cohort with Merkel cell carcinoma.
Asgari MM, Sokil MM, Warton EM, Iyer J, Paulson KG, Nghiem P.
JAMA Dermatol. 2014 Jul;150(7):716-23.
PMID: 24807619
Abstract and Highlights
- IMPORTANCE: Merkel cell carcinoma (MCC) is a rare, aggressive, neuroendocrine-derived skin cancer with high rates of recurrence and associated mortality. Few published studies have used comprehensive patient data and long-term follow-up to examine factors that predict MCC outcomes.
- OBJECTIVE: To characterize MCC in a large defined-population cohort and analyze predictors of disease recurrence and survival.
- SETTING, DESIGN, AND PARTICIPANTS: Retrospective cohort study of 218 patients with MCC from the cancer registry of Kaiser Permanente Northern California, a large integrated health care delivery system. Patients were diagnosed as having MCC and followed up from January 1, 1995, through December 31, 2009. We examined host (age, sex, race, and immunosuppression), tumor (anatomic site, size, and extent), diagnostic (results of imaging and pathologic nodal evaluation), and treatment (surgery, radiation therapy, and chemotherapy) variables for their association with MCC outcomes.
- EXPOSURE: Host, tumor, diagnostic, and treatment factors.
- MAIN OUTCOMES AND MEASURES: Recurrence (locoregional and distant) of MCC and patient survival (overall and MCC specific).
- RESULTS: We estimated adjusted hazard ratios (AHRs) and 95% CIs for outcomes using Cox proportional hazards regression models. After adjustment for host, tumor, diagnostic, and treatment variables, tumor extent (categorized as local, regional, and distant) remained significantly associated with all outcomes. Immunosuppression was associated with higher MCC-specific mortality (AHR, 4.9 [95% CI, 1.7-14.4]), and an unknown primary site was associated with a lower risk for distant metastasis (0.1 [0.0-0.7]) and improved survival (0.4 [0.2-0.9]). Pathological nodal evaluation was associated with a lower risk for metastasis (AHR, 0.2 [95% CI, 0.0-1.0]) and improved survival. Radiation treatment was associated with a decreased risk for locoregional recurrence (AHR, 0.3 [95% CI, 0.1-0.6]), whereas chemotherapy was not associated with any alteration in outcomes.
- CONCLUSIONS AND RELEVANCE: Tumor site and extent, results of pathologic nodal evaluation, and the presence of radiation treatment were associated with MCC recurrence. Immunosuppression, tumor extent, and results of pathologic nodal evaluation were associated with MCC-specific survival, whereas chemotherapy was not associated with any outcomes. Our findings may help to inform diagnostic and therapeutic management of MCCs.
Inhibition of UVB-induced nonmelanoma skin cancer: a path from tea to caffeine to exercise to decreased tissue fat.
Conney AH, Lou YR, Nghiem P, Bernard JJ, Wagner GC, Ju YP.
Top Curr Chem. 2013;329:61-72.
PMID: 22752580
Abstract and Highlights
- Oral administration of green tea, black tea, or caffeine (but not the decaffeinated teas) inhibited ultraviolet B radiation (UVB)-induced skin carcinogenesis in SKH-1 mice. Studies with caffeine indicated that its inhibitory effect on the ATR/Chk1 pathway is an important mechanism for caffeine’s inhibition of UVB-induced carcinogenesis. The regular teas or caffeine increased locomotor activity and decreased tissue fat. In these studies, decreased dermal fat thickness was associated with a decrease in the number of tumors per mouse. Administration of caffeine, voluntary exercise, and removal of the parametrial fat pads all stimulated UVB-induced apoptosis, inhibited UVB-induced carcinogenesis, and stimulated apoptosis in UVB-induced tumors. These results suggest that caffeine administration, voluntary exercise, and removal of the parametrial fat pads inhibit UVB-induced carcinogenesis by stimulating UVB-induced apoptosis and by enhancing apoptosis in DNA-damaged precancer cells and in cancer cells. We hypothesize that tissue fat secretes antiapoptotic adipokines that have a tumor promoting effect.
T-cell Responses to Oncogenic Merkel Cell Polyomavirus Proteins Distinguish Patients with Merkel Cell Carcinoma from Healthy Donors.
Lyngaa R, Pedersen NW, Schrama D, Thrue CA, Ibrani D, Met Ö, Thor Straten P, Nghiem P, Becker JC, Hadrup SR.
Clin Cancer Res. 2014 Apr 1;20(7):1768-78.
PMID: 24526738
Abstract and Highlights
- PURPOSE: Merkel cell carcinoma (MCC) is a highly aggressive skin cancer with strong evidence of viral carcinogenesis. The association of MCC with the Merkel cell polyomavirus (MCPyV) may explain the explicit immunogenicity of MCC. Indeed, MCPyV-encoded proteins are likely targets for cytotoxic immune responses to MCC as they are both foreign to the host and necessary to maintain the oncogenic phenotype. However, to date only a single MCPyV-derived CD8 T-cell epitope has been described, thus impeding specific monitoring of T-cell responses to MCC.
- METHOD: To overcome this limitation, we scanned the MCPyV oncoprotein large T and small T antigens and the virus capsid protein VP1 for potential T-cell epitopes, and tested for MHC class I affinity. We confirmed the relevance of these epitopes using a high-throughput platform for T-cell enrichment and combinatorial encoding of MHC class I multimers.
- RESULTS: In peripheral blood from 38 patients with MCC and 30 healthy donors, we identified 53 MCPyV-directed CD8 T-cell responses against 35 different peptide sequences. Strikingly, T-cell responses against oncoproteins were exclusively present in patients with MCC, but not in healthy donors. We further demonstrate both the processing and presentation of the oncoprotein-derived epitopes, as well as the lytic activity of oncoprotein-specific T cells toward MHC-matched MCC cells. Demonstrating the presence of oncoprotein-specific T cells among tumor-infiltrating lymphocytes further substantiated the relevance of the identified epitopes.
- CONCLUSION: These T-cell epitopes represent ideal targets for antigen-specific immune therapy of MCC, and enable tracking and characterization of MCPyV-specific immune responses.
Relationships among primary tumor size, number of involved nodes, and survival for 8044 cases of Merkel cell carcinoma.
Iyer, JG, Storer, BE, Paulson, KG, Lemos, B, Phillips, JL, Bichakjian C, Zeitouni N, Gershenwald JE, Sondak V, Otley CC, Yu SS, Johnson TM, Liegeois NJ, Byrd D, Sober A, Nghiem P
J Am Acad Dermatol. 2014 Apr;70(4):637-643.
PMID: 24521828
Abstract and Highlights
- BACKGROUND: The effects of primary tumor size on nodal involvement and of number of involved nodes on survival have not, to our knowledge, been examined in a national database of Merkel cell carcinoma (MCC).
- OBJECTIVE: We sought to analyze a retrospective cohort of patients with MCC from the largest US national database to assess the relationships between these clinical parameters and survival.
- METHODS: A total of 8044 MCC cases in the National Cancer Data Base were analyzed.
- RESULTS: There was a 14% risk of regional nodal involvement for 0.5-cm tumors that increased to 25% for 1.7-cm (median-sized) tumors and to more than 36% for tumors 6 cm or larger. The number of involved nodes was strongly predictive of survival (0 nodes, 76% 5-year relative survival; 1 node, 50%; 2 nodes, 47%; 3-5 nodes, 42%; and ≥6 nodes, 24%; P < .0001 for trend). Younger and/or male patients were more likely to undergo pathological nodal evaluation.
- LIMITATIONS: The National Cancer Data Base does not capture disease-specific survival. Hence, relative survival was calculated by comparing overall survival with age- and sex-matched US population data.
- CONCLUSION: Pathologic nodal evaluation should be considered even for patients with small primary MCC tumors. The number of involved nodes is strongly predictive of survival and may help improve prognostic accuracy and management.
Clinical utility of a circulating tumor cell assay in Merkel cell carcinoma.
Blom A, Bhatia S, Pietromonaco S, Koehler K, Iyer JG, Nagase K, Paulson K, Sabath DE, Nghiem P.
J Am Acad Dermatol. 2014 Mar;70(3):449-55.
PMID: 24388423
Abstract and Highlights
- BACKGROUND: Quantitation of circulating tumor cells (CTCs) has utility in managing breast, colon, and prostate carcinomas.
- OBJECTIVE: We sought to determine whether a commercially available CTC assay provides prognostic information in Merkel cell carcinoma (MCC), insight into treatment responses, or both.
- METHODS: We analyzed CTCs in 52 specimens from 34 patients with MCC.
- RESULTS: The presence of CTCs correlated with extent of disease at blood draw (P = .004). Among 15 patients with regional nodal disease, CTC-negative patients had 80% disease-specific survival at 2 years after the test, versus 29% for CTC-positive patients (P = .015). Among the entire cohort, those without CTCs had 72% MCC-specific survival whereas CTC-positive patients had 25% survival (n = 34, median follow-up 19 months, P = .0003). Fifty seven percent of patients with MCC had a cytokeratin “dot” visible in 20% or more of CTCs, a feature that was absent among CTCs from other carcinomas (0 of 13 cases).
- LIMITATIONS: CTC assay was performed at variable times after diagnosis and heterogeneity in extent of disease affects interpretability of the data.
- CONCLUSION: CTC detection in MCC is feasible and appears to add prognostic information, particularly in patients with regional nodal disease. It may also assist clinical management in certain situations, including differentiating metastatic MCC cells from those of other carcinomas.
Merkel cell carcinoma, version 1.2014.
Bichakjian CK, Olencki T, Alam M, Andersen JS, Berg D, Bowen GM, Cheney RT, Daniels GA, Glass LF, Grekin RC, Grossman K, Ho AL, Lewis KD, Lydiatt DD, Morrison WH, Nehal KS, Nelson KC, Nghiem P, Perlis CS, Shaha AR, Thorstad WL, Tuli M, Urist MM, Wang TS, Werchniak AE, Wong SL, Zic JA, Hoffmann KG, McMillian NR, Ho M.
J Natl Compr Canc Netw. 2014 Mar 1;12(3):410-24.
PMID: 24616545
Abstract and Highlights
- Merkel cell carcinoma is a rare, aggressive cutaneous tumor that combines the local recurrence rates of infiltrative nonmelanoma skin cancer with the regional and distant metastatic rates of thick melanoma. The NCCN Guidelines for Merkel Cell Carcinoma provide recommendations on the diagnosis and management of this aggressive disease based on clinical evidence and expert consensus. This version includes revisions regarding the use of PET/CT imaging and the addition of a new section on the principles of pathology to provide guidance on the analysis, interpretation, and reporting of pathology results.
Regression of metastatic Merkel cell carcinoma following transfer of polyomavirus-specific T cells and therapies capable of reinducing HLA class-I.
Chapuis AG, Afanasiev OK, Iyer JG, Paulson KG, Parvathaneni U, Hwang JH, Lai I, Roberts IM, Sloan HL, Bhatia S, Shibuya KC, Gooley T, Desmarais C, Koelle DM, Yee C, Nghiem P.
Cancer Immunol Res. 2014 Jan;2(1):27-36.
PMID: 24432305
Abstract and Highlights
- Merkel cell carcinoma (MCC) is an aggressive skin cancer that typically requires the persistent expression of Merkel cell polyomavirus (MCPyV) oncoproteins that can serve as ideal immunotherapeutic targets. Several immune evasion mechanisms are active in MCC including down-regulation of HLA class-I expression on tumor cells and dysfunctional endogenous MCPyV-specific CD8 T cell responses. To overcome these obstacles, we combined local and systemic immune therapies in a 67-year-old man, who developed metastatic MCPyV-expressing MCC. Intralesional IFNβ-1b or targeted single-dose radiation was administered as a pre-conditioning strategy to reverse the down-regulation of HLA-I expression noted in his tumors and to facilitate the subsequent recognition of tumor cells by T cells. This was followed by the adoptive transfer of ex vivo expanded polyclonal, polyomavirus-specific T cells as a source of reactive antitumor immunity. The combined regimen was well-tolerated and led to persistent up-regulation of HLA-I expression in the tumor and a durable complete response in two of three metastatic lesions. Relative to historical controls, the patient experienced a prolonged period without development of additional distant metastases (535 days compared to historic median of 200 days, 95% confidence interval = 154-260 days). The transferred CD8(+) T cells preferentially accumulated in the tumor tissue, remained detectable and functional for >200 days, persisted with an effector phenotype, and exhibited evidence of recent in vivo activation and proliferation. The combination of local and systemic immune stimulatory therapies was well-tolerated and may be a promising approach to overcome immune evasion in virus-driven cancers.
Pathogen-driven cancers and emerging immune therapeutic strategies.
Vandeven N, Nghiem P.
Cancer Immunol Res. 2014 Jan;2(1):9-14.
PMID: 24778160
Abstract and Highlights
- Infectious agents play an etiologic role in approximately 20% of cancer cases worldwide. Eleven pathogens (seven viruses, three parasites, and one bacterium) are known to contribute to oncogenesis either directly via the expression of their protein products or indirectly via chronic inflammation. Although prevention of infection and antimicrobial treatments have helped in reducing infection rates and the incidence of associated malignancies, therapies for these cancers remain limited. The importance of immune control over malignant progression is highlighted by the fact that many cancers, particularly those induced by pathogens, occur more frequently among immunosuppressed patients as compared with healthy individuals. Therefore, therapeutic strategies that can elicit a robust immune response and restore tumor detection may be a beneficial approach for treating these cancers. In addition, the study of immune escape mechanisms used by pathogens and their associated cancers may provide insight into the mechanisms of malignant transformation and improved therapies for cancer more generally.
2013
Immunobiology of Merkel cell carcinoma: implications for immunotherapy of a polyomavirus-associated cancer.
Bhatia S, Afanasiev O, Nghiem P.
Curr Oncol Rep. 2011 Dec;13(6):488-97.
PMID: 21953511
Abstract and Highlights
- Merkel cell carcinoma (MCC) is an aggressive skin malignancy with a high mortality rate and an increasing incidence. The recent discovery of Merkel cell polyomavirus has revolutionized our understanding of MCC pathogenesis. Viral oncoproteins appear to play a critical role in tumor progression and are expressed in the majority of MCC tumors. Virus-specific humoral and cellular immune responses are detectable in MCC patients and are linked to the natural history of the disease. Despite persistent expression of immunogenic viral proteins, however, MCC tumors are able to evade the immune system. Understanding of the mechanisms of immune evasion employed by MCC tumors is rapidly increasing and offers opportunities for development of rational immune therapies to improve patient outcomes. Here we review recent discoveries in MCC with a special focus on the pathogenic role of Merkel cell polyomavirus and the immunobiology of this virus-associated disease.
Mechanisms of caffeine-induced inhibition of UVB carcinogenesis.
Conney AH, Lu Y-P, Lou Y-R, Kawasumi M, Nghiem P.
Front Oncol. 2013 Jun 17;3:144.
PMID: 23785666
Abstract and Highlights
- Sunlight-induced non-melanoma skin cancer is the most prevalent cancer in the United States with more than two million cases per year. Several studies have shown an inhibitory effect of caffeine administration on UVB-induced skin cancer in mice, and these studies are paralleled by epidemiology studies that indicate an inhibitory effect of coffee drinking on non-melanoma skin cancer in humans. Strikingly, decaffeinated coffee consumption had no such inhibitory effect. Mechanism studies indicate that caffeine has a sunscreen effect that inhibits UVB-induced formation of thymine dimers and sunburn lesions in the epidermis of mice. In addition, caffeine administration has a biological effect that enhances UVB-induced apoptosis thereby enhancing the elimination of damaged precancerous cells, and caffeine administration also enhances apoptosis in tumors. Caffeine administration enhances UVB-induced apoptosis by p53-dependent and p53-independent mechanisms. Exploration of the p53-independent effect indicated that caffeine administration enhanced UVB-induced apoptosis by inhibiting the UVB-induced increase in ATR-mediated formation of phospho-Chk1 (Ser345) and abolishing the UVB-induced decrease in cyclin B1 which resulted in caffeine-induced premature and lethal mitosis in mouse skin. In studies with cultured primary human keratinocytes, inhibition of ATR with siRNA against ATR inhibited Chk1 phosphorylation and enhanced UVB-induced apoptosis. Transgenic mice with decreased epidermal ATR function that were irradiated chronically with UVB had 69% fewer tumors at the end of the study compared with irradiated littermate controls with normal ATR function. These results, which indicate that genetic inhibition of ATR (like pharmacologic inhibition of ATR via caffeine) inhibits UVB-induced carcinogenesis support the concept that ATR-mediated phosphorylation of Chk1 is an important target for caffeine’s inhibitory effect on UVB-induced carcinogenesis.
Emerging and mechanism-based therapies for recurrent or metastatic Merkel cell carcinoma.
Miller NJ, Bhatia S, Parvathaneni U, Iyer JG, Nghiem P.
Curr Treat Options Oncol. 2013 Jun;14(2):249-63.
PMID: 23436166
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a rare but aggressive neuroendocrine skin cancer with a disease-specific mortality of approximately 40 %. The association of MCC with a recently discovered polyomavirus, combined with the increased incidence and mortality of MCC among immunocompromised patients, highlight the importance of the immune system in controlling this cancer. Initial management of MCC is summarized within the NCCN guidelines and in recently published reviews. The high rate of recurrent and metastatic disease progression in MCC, however, presents a major challenge in a cancer that lacks mechanism-based, disease-specific therapies. Traditional treatment approaches have focused on cytotoxic chemotherapy that, despite frequent initial efficacy, rarely provides durable responses and has high morbidity among the elderly. In addition, the immunosuppressive nature of chemotherapy is of concern when treating a virus-associated cancer for which survival is unusually tightly linked to immune function. With a median survival of 9.6 months after development of an initial metastasis (n = 179, described herein), and no FDA-approved agents for this cancer, there is an urgent need for more effective treatments. We review diverse management options for patients with advanced MCC, with a focus on emerging and mechanism-based therapies, some of which specifically target persistently expressed viral antigens. These treatments include single-dose radiation and novel immunotherapies, some of which are in clinical trials. Due to their encouraging efficacy, low toxicity, and lack of immune suppression, these therapies may offer viable alternatives to traditional cytotoxic chemotherapy.
Merkel cell polyomavirus large T antigen has growth promoting and inhibitory activities.
Cheng J, Rozenblatt-Rosen O, Paulson KG, Nghiem P, DeCaprio JA.
J Virol. 2013 Jun;87(11):6118-26.
PMID: 23514892
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a rare and aggressive form of skin cancer. In at least 80% of all MCC, Merkel cell polyomavirus (MCPyV) DNA has undergone clonal integration into the host cell genome, and most tumors express the MCPyV large and small T antigens. In all cases of MCC reported to date, the integrated MCPyV genome has undergone mutations in the large T antigen. These mutations result in expression of a truncated large T antigen that retains the Rb binding or LXCXE motif but deletes the DNA binding and helicase domains. However, the transforming functions of full-length and truncated MCPyV large T antigen are unknown. We compared the transforming activities of full-length, truncated, and alternatively spliced 57kT forms of MCPyV large T antigen. MCPyV large T antigen could bind to Rb but was unable to bind to p53. Furthermore, MCPyV-truncated large T antigen was more effective than full-length and 57kT large T antigen in promoting the growth of human and mouse fibroblasts. In contrast, expression of the MCPyV large T antigen C-terminal 100 residues could inhibit the growth of several different cell types. These data imply that the deletion of the C terminus of MCPyV large T antigen found in MCC serves not only to disrupt viral replication but also results in the loss of a distinct growth-inhibitory function intrinsic to this region.
p63 expression in Merkel cell carcinoma predicts poorer survival yet may have limited clinical utility.
Stetsenko Gy, Malekirad J, Paulson KG, Iyer JG, Thibodeau Rm, Nagase K, Schmidt M, Storer BE, Argenyi ZB, Nghiem P.
Am J Clin Pathol. 2013 Dec;140(6):838-44.
PMID: 24225752
Abstract and Highlights
- OBJECTIVES: To determine the clinical utility of p63 expression, which has been identified in several cohorts as a predictor of poorer prognosis in Merkel cell carcinoma (MCC).
- METHODS: Immunohistochemistry was used to determine p63 expression on MCC tumors from 128 patients.
- RESULTS: Of the patients, 33% had detectable p63 expression. p63 Positivity was associated with an increased risk of death from MCC (hazard ratio, 2.05; P = .02) in a multivariate Cox regression model considering stage at presentation, age at diagnosis, and sex. Although p63 expression correlated with diminished survival in this largest cohort reported thus far, the effect was weaker than that observed in prior studies. Indeed, within a given stage, p63 status did not predict survival in a clinically or statistically significant manner.
- CONCLUSIONS: It remains unclear whether this test should be integrated into routine MCC patient management.
Merkel cell polyomavirus-specific T cells fluctuate with Merkel cell carcinoma burden and express therapeutically targetable PD-1 and Tim-3 exhaustion markers.
Afanasiev OK, Yelistratova L, Miller N, Nagase K, Paulson KG, Iyer JG, Ibrani D, Koelle DM, Nghiem P.
Clin Cancer Res. 2013 Oct 1;19(19):5351-60.
PMID: 23922299
Abstract and Highlights
- PURPOSE: The persistent expression of Merkel cell polyomavirus (MCPyV) oncoproteins in Merkel cell carcinoma (MCC) provides a unique opportunity to characterize immune evasion mechanisms in human cancer. We isolated MCPyV-specific T cells and determined their frequency and functional status.
- EXPERIMENTAL DESIGN: Multiparameter flow cytometry panels and HLA/peptide tetramers were used to identify and characterize T cells from tumors (n = 7) and blood (n = 18) of patients with MCC and control subjects (n = 10). PD-1 ligand (PD-L1) and CD8 expression within tumors were determined using mRNA profiling (n = 35) and immunohistochemistry (n = 13).
- RESULTS: MCPyV-specific CD8 T cells were detected directly ex vivo from the blood samples of 7 out of 11 (64%) patients with MCPyV-positive tumors. In contrast, 0 of 10 control subjects had detectable levels of these cells in their blood (P < 0.01). MCPyV-specific T cells in serial blood specimens increased with MCC disease progression and decreased with effective therapy. MCPyV-specific CD8 T cells and MCC-infiltrating lymphocytes expressed higher levels of therapeutically targetable PD-1 and Tim-3 inhibitory receptors compared with T cells specific to other human viruses (P < 0.01). PD-L1 was present in 9 of 13 (69%) MCCs and its expression was correlated with CD8-lymphocyte infiltration.
- CONCLUSIONS: MCC-targeting T cells expand with tumor burden and express high levels of immune checkpoint receptors PD-1 and Tim-3. Reversal of these inhibitory pathways is therefore a promising therapeutic approach for this virus-driven cancer.
Pathologic nodal evaluation is increasingly commonly performed for patients with Merkel cell carcinoma.
Paulson KG, Iyer JG, Byrd DR, Nghiem P.
J Am Acad Dermatol. 2013 Oct;69(4):653-4.
PMID: 24034376
Vascular E-selectin expression correlates with CD8 lymphocyte infiltration and improved outcome in Merkel cell carcinoma.
Afanasiev OK, Nagase K, Simonson W, Vandeven N, Blom A, Koelle DM, Clark R, Nghiem P.
J Invest Dermatol. 2013 Aug;133(8):2065-73.
PMID: 23353989
Abstract and Highlights
- Merkel cell carcinoma (MCC) is an aggressive, polyomavirus-linked skin cancer. Although CD8 lymphocyte infiltration into the tumor is strongly correlated with improved survival, these cells are absent or sparse in most MCCs. We investigated whether specific mechanisms of T-cell migration may be commonly disrupted in MCC tumors with poor CD8 lymphocyte infiltration. Intratumoral vascular E-selectin, critical for T-cell entry into skin, was downregulated in the majority (52%) of MCCs (n=56), and its loss was associated with poor intratumoral CD8 lymphocyte infiltration (P<0.05; n=45). Importantly, survival was improved in MCC patients whose tumors had higher vascular E-selectin expression (P<0.05). Local nitric oxide (NO) production is one mechanism of E-selectin downregulation and it can be tracked by quantifying nitrotyrosine, a stable biomarker of NO-induced reactive nitrogen species (RNS). Indeed, increasing levels of nitrotyrosine within MCC tumors were associated with low E-selectin expression (P<0.05; n=45) and decreased CD8 lymphocyte infiltration (P<0.05, n=45). These data suggest that one mechanism of immune evasion in MCC may be restriction of T-cell entry into the tumor. Existing therapeutic agents that modulate E-selectin expression and/or RNS generation may restore T-cell entry and could potentially synergize with other immune-stimulating therapies.
Tumor-specific T cells in human Merkel cell carcinomas: a possible role for Tregs and T cell exhaustion in reducing T cell responses.
Dowlatshahi M, Huang V, Gehad A, Jiang Y, Calarese A, Teague JE, Dorosario A, Cheng J, Nghiem P, Schanbacher C, Thakuria M, Schmults C, Wang LC, Clark RA.
J Invest Dermatol. 2013 Jul;133(7):1879-89.
PMID: 23419694
Abstract and Highlights
- Merkel cell carcinomas (MCCs) are rare but highly malignant skin cancers associated with a recently described polyomavirus. MCC tumors were infiltrated by T cells, including effector, central memory, and regulatory T cells. Infiltrating T cells showed markedly reduced activation as evidenced by reduced expression of CD69 and CD25. Treatment of MCC tumors in vitro with IL-2 and IL-15 led to T-cell activation, proliferation, enhanced cytokine production, and loss of viable tumor cells from cultures. Expanded tumor-infiltrating lymphocytes showed TCR repertoire skewing and upregulation of CD137. MCC tumors implanted into immunodeficient mice failed to grow unless human T cells in the tumor grafts were depleted with denileukin diftitox, suggesting that tumor-specific T cells capable of controlling tumor growth were present in MCC. Both CD4(+) and CD8(+) FOXP3(+) regulatory T cells were frequent in MCC. Fifty percent of nonactivated T cells in MCC-expressed PD-1, a marker of T-cell exhaustion, and PD-L1 and PD-L2 were expressed by a subset of tumor dendritic cells and macrophages. In summary, we observed tumor-specific T cells with suppressed activity in MCC tumors. Agents that stimulate T-cell activity, block regulatory T cell function, or inhibit PD-1 signaling may be effective in the treatment of this highly malignant skin cancer.
Systemic immune suppression predicts diminished Merkel cell carcinoma-specific survival independent of stage.
Paulson KG, Iyer JG, Blom A, Warton EM, Sokil M, Yelistratova L, Schuman L Nagase K, Bhatia S, Asgari MM, Nghiem P.
J Invest Dermatol. 2013 Mar;133(3):642-646.
PMID: 23190897
Abstract and Highlights
- Merkel cell carcinoma (MCC) is an aggressive cutaneous malignancy linked to a contributory virus (Merkel cell polyomavirus). Multiple epidemiologic studies have established an increased incidence of MCC among persons with systemic immune suppression. Several forms of immune suppression are associated with increased MCC incidence, including hematologic malignancies, HIV/AIDS, and immunosuppressive medications for autoimmune disease or transplant. Indeed, immune-suppressed individuals represent ∼10% of MCC patients, a significant overrepresentation relative to the general population. We hypothesized that immune-suppressed patients may have a poorer MCC-specific prognosis and examined a cohort of 471 patients with a combined follow-up of 1,427 years (median 2.1 years). Immune-suppressed patients (n=41) demonstrated reduced MCC-specific survival (40% at 3 years) compared with patients with no known systemic immune suppression (n=430; 74% MCC-specific survival at 3 years). By competing risk regression analysis, immune suppression was a stage-independent predictor of worsened MCC-specific survival (hazard ratio 3.8, P<0.01). Thus, immune-suppressed individuals have both an increased chance of developing MCC and poorer MCC-specific survival. It may be appropriate to follow these higher-risk individuals more closely, and, when clinically feasible, there may be a benefit of diminishing iatrogenic systemic immune suppression.
2012
Complete Spontaneous Regression of Merkel Cell Carcinoma Metastatic to the Liver: Did Lifestyle Modifications and Dietary Supplements Play a Role?
Vandeven N, Nghiem P.
Glob Adv Health Med. 2012 Nov;1(5):22-3.
PMID: 27257527
Importance of genetic studies in patients with multiple merkel cell carcinomas.
Ahronowitz I, Nghiem P, Yu S.
Acta Derm Venereol. 2012 Nov;92(6):633; author reply p.634.
PMID: 22334083
Abstract and Highlights
Metachronous Merkel cell carcinoma on both cheeks.
Diagnostic biopsy does not commonly induce intratumoral CD8 T cell infiltration in Merkel cell carcinoma.
Koba S, Paulson KG, Nagase K, Tegeder A, Thibodeau R, Iyer JG, Narisawa Y, Nghiem P.
PLoS One. 2012;7(7):e41465.
PMID: 22859987
Abstract and Highlights
- BACKGROUND: Merkel cell carcinoma is a polyomavirus-associated cancer that is strongly linked with T lymphocyte immune suppression in epidemiologic studies. CD8+ T cell infiltration into MCC tumors (intratumoral) has recently been shown to be strongly predictive of improved survival. In contrast, the presence of CD8+ T cells at the border of the tumor (peritumoral) had no independent prognostic value. Spontaneous regression has been reported for MCC approximately one thousand times more often than would be expected given the frequency of this cancer. Many of these events began shortly after biopsy, and in some cases lymphocytic infiltration was described.
- METHODOLOGY/PRINCIPAL FINDINGS: To determine whether CD8+ lymphocyte infiltration in MCC tumors is commonly altered by biopsy.33 MCC patients who had microscopic confirmation of MCC on both an initial biopsy and a re-excision specimen were included in this study. Intratumoral and peritumoral CD8 lymphocyte infiltration was quantitated using immunohistochemistry and compared using the paired t-test in biopsy versus re-excision samples. There was a trend toward increased CD8 infiltration after biopsy in a peritumoral (‘stalled’) pattern (p = 0.08), however, biopsy was not associated with a significant increase in CD8 T cells in the clinically more important intratumoral location (p = 0.58).
- CONCLUSIONS/SIGNIFICANCE: The initial diagnostic biopsy for MCC does not commonly alter intratumoral CD8+ T cell infiltration, suggesting it does not directly induce immunologic recognition of this cancer. Because CD8 infiltration is typically stable after biopsy, this parameter may be useful to assess the efficacy of future immune therapies for this virus-associated, immunogenic, often-lethal cancer.
Surgical removal of the parametrial fat pads stimulates apoptosis and inhibits UVB-induced carcinogenesis in mice fed a high-fat diet.
Lu YP, Lou YR, Bernard JJ, Peng QY, Li T, Lin Y, Shih WJ, Nghiem P, Shapses S, Wagner GC, Conney AH.
Proc Natl Acad Sci U S A. 2012 Jun 5;109(23):9065-70.
PMID: 22615388
Abstract and Highlights
- Removal of the parametrial fat pads (partial lipectomy) from female SKH-1 mice fed a high-fat diet inhibited UVB-induced carcinogenesis, but this was not observed in mice fed a low-fat chow diet. Partial lipectomy in high-fat-fed mice decreased the number of keratoacanthomas and squamous cell carcinomas per mouse by 76 and 79%, respectively, compared with sham-operated control mice irradiated with UVB for 33 wk. Immunohistochemical analysis indicated that partial lipectomy increased caspase 3 (active form) positive cells by 48% in precancerous epidermis away from tumors, by 68% in keratoacanthomas, and by 224% in squamous cell carcinomas compared with sham-operated control mice. In addition, partial lipectomy decreased cell proliferation away from tumors and in tumors. RT-PCR analysis for adipokines revealed that mRNAs for TIMP1, MCP1, and SerpinE1 (proinflammatory/antiapoptotic cytokines) in the parametrial fat pads of sham-operated control mice were 54- to 83-fold higher than levels in compensatory fat that returned after surgery in partially lipectomized mice at the end of the tumor study. Feeding mice high-fat diets for 2 wk increased levels of TIMP1 and other adipokines in serum and epidermis, and these increases were inhibited by removal of the parametrial fat pads. Our results are a unique demonstration that surgical removal of a specific tissue fat results in inhibition of carcinogenesis in obese mice. This inhibition was associated with an increase in apoptosis and a decrease in proliferation in tumors and in precancerous areas away from tumors.
2011
Left-sided skin cancers on the arm from driving? Past and future lessons from Australia.
Paulson K, Iyer J, Nghiem P.
J Am Acad Dermatol. 2011 Dec;65(6):1229.
PMID: 22082843
A new American Joint Committee on Cancer staging system for cutaneous squamous cell carcinoma: Creation and rationale for inclusion of tumor (T) characteristics.
Farasat S, Yu SS, Neel VA, Nehal KS, Lardaro T, Mihm MC, Byrd DR, Balch CM, Califano JA, Chuang AY, Sharfman WH, Shah JP, Nghiem P, Otley CC, Tufaro AP, Johnson TM, Sober AJ, Liégeois NJ.
J Am Acad Dermatol. 2011 Jun;64(6):1051-9.
PMID: 21255868
Abstract and Highlights
- BACKGROUND: The incidence of cutaneous squamous cell carcinoma (cSCC) is increasing. Although most patients achieve complete remission with surgical treatment, those with advanced disease have a poor prognosis. The American Joint Committee on Cancer (AJCC) is responsible for the staging criteria for all cancers. For the past 20 years, the AJCC cancer staging manual has grouped all nonmelanoma skin cancers, including cSCC, together for the purposes of staging. However, based on new evidence, the AJCC has determined that cSCC should have a separate staging system in the 7th edition AJCC staging manual.
- OBJECTIVE: We sought to present the rationale for and characteristics of the new AJCC staging system specific to cSCC tumor characteristics (T).
- METHODS: The Nonmelanoma Skin Cancer Task Force of AJCC reviewed relevant data and reached expert consensus in creating the 7th edition AJCC staging system for cSCC. Emphasis was placed on prospectively accumulated data and multivariate analyses. Concordance with head and neck cancer staging system was also achieved.
- RESULTS: A new AJCC cSCC T classification is presented. The T classification is determined by tumor diameter, invasion into cranial bone, and high-risk features, including anatomic location, tumor thickness and level, differentiation, and perineural invasion.
- LIMITATIONS: The data available for analysis are still suboptimal, with limited prospective outcomes trials and few multivariate analyses.
- CONCLUSIONS: The new AJCC staging system for cSCC incorporates tumor-specific (T) staging features and will encourage coordinated, consistent collection of data that will be the basis of improved prognostic systems in the future.
Identification and validation of a novel mature microRNA encoded by the Merkel cell polyomavirus in human Merkel cell carcinomas.
Lee S, Paulson KG, Murchison EP, Afanasiev OK, Alkan C, Leonard JH, Byrd DR, Hannon GJ, Nghiem PT.
J Clin Virol. 2011 Nov;52(3):272-5.
PMID: 21907614
Abstract and Highlights
- BACKGROUND: Merkel cell polyomavirus (MCPyV) is present in approximately 80% of human Merkel cell carcinomas (MCCs). A previous in silico prediction suggested MCPyV encodes a microRNA (miRNA) that may regulate cellular and viral genes.
- OBJECTIVES: To determine the presence and prevalence of a putative MCPyV-encoded miRNA in human MCC tumors.
- STUDY DESIGN: Over 30 million small RNAs from 7 cryopreserved MCC tumors and 1 perilesional sample were sequenced. 45 additional MCC tumors were examined for expression of an MCPyV-encoded mature miRNA by reverse transcription real-time PCR.
- RESULTS: An MCPyV-encoded mature miRNA, “MCV-miR-M1-5p”, was detected by direct sequencing in 2 of 3 MCPyV-positive MCC tumors. Although a precursor miRNA, MCV-miR-M1, had been predicted in silico and studied in vitro by Seo et al., no MCPyV-encoded miRNAs have been directly detected in human tissues. Importantly, the mature sequence of MCV-miR-M1 found in vivo was identical in all 79 reads obtained but differed from the in silico predicted mature miRNA by a 2-nucleotide shift, resulting in a distinct seed region and a different set of predicted target genes. This mature miRNA was detected by real-time PCR in 50% of MCPyV-positive MCCs (n = 38) and in 0% of MCPyV-negative MCCs (n = 13).
- CONCLUSIONS: MCV-miR-M1-5p is expressed at low levels in 50% of MCPyV-positive MCCs. This virus-encoded miRNA is predicted to target genes that may play a role in promoting immune evasion and regulating viral DNA replication.
Merkel cell polyomavirus-specific CD8+ and CD4+ T-cell responses identified in Merkel cell carcinomas and blood.
Iyer JG, Afanasiev OK, McClurkan C, Paulson KG, Nagase K, Jing L, Marshak J, Dong L, Carter JJ, Lai I, Farrar E, Byrd D, Galloway D, Yee C, Koelle DM, Nghiem P.
Clin Cancer Res. 2011 Nov 1;17(21):6671-80.
PMID: 21908576
Abstract and Highlights
- PURPOSE: Merkel cell polyomavirus (MCPyV) is prevalent in the general population, integrates into most Merkel cell carcinomas (MCC), and encodes oncoproteins required for MCC tumor growth. We sought to characterize T-cell responses directed against viral proteins that drive this cancer as a step toward immunotherapy.
- EXPERIMENTAL DESIGN: Intracellular cytokine cytometry, IFN-γ enzyme-linked immunospot (ELISPOT) assay, and a novel HLA-A*2402-restricted MCPyV tetramer were used to identify and characterize T-cell responses against MCPyV oncoproteins in tumors and blood of MCC patients and control subjects.
- RESULTS: We isolated virus-reactive CD8 or CD4 T cells from MCPyV-positive MCC tumors (2 of 6) but not from virus-negative tumors (0 of 4). MCPyV-specific T-cell responses were also detected in the blood of MCC patients (14 of 27) and control subjects (5 of 13). These T cells recognized a broad range of peptides derived from capsid proteins (2 epitopes) and oncoproteins (24 epitopes). HLA-A*2402-restricted MCPyV oncoprotein processing and presentation by mammalian cells led to CD8-mediated cytotoxicity. Virus-specific CD8 T cells were markedly enriched among tumor infiltrating lymphocytes as compared with blood, implying intact T-cell trafficking into the tumor. Although tetramer-positive CD8 T cells were detected in the blood of 2 of 5 HLA-matched MCC patients, these cells failed to produce IFN-γ when challenged ex vivo with peptide.
- CONCLUSIONS: Our findings suggest that MCC tumors often develop despite the presence of T cells specific for MCPyV T-Ag oncoproteins. The identified epitopes may be candidates for peptide-specific vaccines and tumor- or virus-specific adoptive immunotherapies to overcome immune evasion mechanisms in MCC patients.
Protection from UV-induced skin carcinogenesis by genetic inhibition of the ataxia telangiectasia and Rad3-related (ATR) kinase.
Kawasumi M, Lemos B, Bradner JE, Thibodeau R, Kim YS, Schmidt M, Higgins E, Koo SW, Angle-Zahn A, Chen A, Levine D, Nguyen L, Heffernan TP, Longo I, Mandinova A, Lu YP, Conney AH, Nghiem P.
Proc Natl Acad Sci U S A. 2011 Aug 16;108(33):13716-21.
PMID: 21844338
Abstract and Highlights
- Multiple human epidemiologic studies link caffeinated (but not decaffeinated) beverage intake with significant decreases in several types of cancer, including highly prevalent UV-associated skin carcinomas. The mechanism by which caffeine protects against skin cancer is unknown. Ataxia telangiectasia and Rad3-related (ATR) is a replication checkpoint kinase activated by DNA stresses and is one of several targets of caffeine. Suppression of ATR, or its downstream target checkpoint kinase 1 (Chk1), selectively sensitizes DNA-damaged and malignant cells to apoptosis. Agents that target this pathway are currently in clinical trials. Conversely, inhibition of other DNA damage response pathways, such as ataxia telangiectasia mutated (ATM) and BRCA1, promotes cancer. To determine the effect of replication checkpoint inhibition on carcinogenesis, we generated transgenic mice with diminished ATR function in skin and crossed them into a UV-sensitive background, Xpc(-/-). Unlike caffeine, this genetic approach was selective and had no effect on ATM activation. These transgenic mice were viable and showed no histological abnormalities in skin. Primary keratinocytes from these mice had diminished UV-induced Chk1 phosphorylation and twofold augmentation of apoptosis after UV exposure (P = 0.006). With chronic UV treatment, transgenic mice remained tumor-free for significantly longer (P = 0.003) and had 69% fewer tumors at the end of observation of the full cohort (P = 0.019), compared with littermate controls with the same genetic background. This study suggests that inhibition of replication checkpoint function can suppress skin carcinogenesis and supports ATR inhibition as the relevant mechanism for the protective effect of caffeinated beverage intake in human epidemiologic studies.
Asymmetric lateral distribution of melanoma and Merkel cell carcinoma in the United States.
Paulson KG, Iyer JG, Nghiem P.
J Am Acad Dermatol. 2011 Jul;65(1):35-9.
PMID: 21514002
Abstract and Highlights
- BACKGROUND: A recent report suggested a trend toward more ultraviolet-linked skin cancers arising on the left rather than the right side of the body in the United States.
- OBJECTIVE: We sought to test whether the reported incidences of two ultraviolet-linked skin cancers, malignant melanoma (MM) and Merkel cell carcinoma (MCC), are statistically significantly greater on the left than the right in the United States.
- METHODS: MMs (n = 82,587) and MCCs (n = 2384) occurring on the left or right side of the face, arm, or leg that were reported in the Surveillance, Epidemiology, and End Results registry between 1986 and 2006 were included for analysis.
- RESULTS: MM and MCC were significantly more likely to present on the left than the right (P < .01 for both MM and MCC). In all, 53% of arm melanomas, 51% of facial melanomas, and 52% of leg melanomas presented on the left. A total of 55% of arm MCCs and 52% of facial MCCs presented on the left, whereas leg MCCs were equally distributed.
- LIMITATIONS: National registry data did not provide information regarding sun exposure or driving habits. No equivalent registry data were available for basal or squamous cell carcinoma.
- CONCLUSIONS: Both melanoma and MCC are significantly more likely to arise on the left than the right, and this effect was most prominent on the arm. Driver-side automobile ultraviolet exposure (approximately 5-fold stronger on the left than right arm) is a likely contributing factor. It may be prudent to remind individuals prone to skin cancer to take appropriate sun precautions when driving in an automobile.
Caffeine decreases phospho-Chk1 (Ser317) and increases mitotic cells with cyclin B1 and caspase 3 in tumors from UVB-treated mice.
Lu Y-P, Lou Y-R, Peng Q-Y, Nghiem P, Conney A H.
Cancer Prev Res (Phila). 2011 Jul;4(7):1118-25.
PMID: 21505179
Abstract and Highlights
- Oral administration of caffeine to mice inhibits UVB-induced carcinogenesis, and these results are paralleled by epidemiology studies indicating that caffeinated coffee and tea intake (but not decaffeinated beverage intake) is associated with decreased incidence of nonmelanoma skin cancer. Topical applications of caffeine to the skin of SKH-1 mice that had previously been treated with UVB inhibited subsequent skin tumor development and stimulated apoptosis in tumors but not in nontumor areas of the epidermis. This study sought to determine the basis of these differential effects on tumor versus nontumor sites that can be induced by caffeine, long after all UVB treatment has ceased. The activation status of the ATR/Chk1 pathway in UVB-induced tumors and uninvolved skin was determined by quantitating phospho-Chk1 (Ser317) and induction of lethal mitosis in vivo in the presence and absence of topical caffeine treatment. In the absence of caffeine, we found that UVB-induced tumors often had islands of phospho-Chk1 (Ser317) staining cells that were not present in nontumor areas of the epidermis. Treatment of mice with topical caffeine significantly diminished phospho-Chk1 (Ser317) staining and increased the number of mitotic cells that expressed cyclin B1 and caspase 3 in tumors, consistent with caffeine-induced lethal mitosis selectively in tumors. We hypothesize that compared with adjacent uninvolved skin, UVB-induced skin tumors have elevated activation of, and dependence on, the ATR/Chk1 pathway long after UVB exposure has ceased and that caffeine can induce apoptosis selectively in tumors by inhibiting this pathway and promoting lethal mitosis.
Chemical methodology as a source of small-molecule checkpoint inhibitors and heat shock protein 70 (Hsp70) modulators.
Huryn D, Brodsky J, Brummond K, Chambers P, Eyre B, Ireland A, Kawasumi M, LaPorte M, Lloyd K, Manteau B, Nghiem P, Quade B, Wipf P.
Proc Natl Acad Sci U S A. 2011 Apr 26;108(17):6757-62.
PMID: 21502524
Abstract and Highlights
- Unique chemical methodology enables the synthesis of innovative and diverse scaffolds and chemotypes and allows access to previously unexplored “chemical space.” Compound collections based on such new synthetic methods can provide small-molecule probes of proteins and/or pathways whose functions are not fully understood. We describe the identification, characterization, and evolution of two such probes. In one example, a pathway-based screen for DNA damage checkpoint inhibitors identified a compound, MARPIN (ATM and ATR pathway inhibitor) that sensitizes p53-deficient cells to DNA-damaging agents. Modification of the small molecule and generation of an immobilized probe were used to selectively bind putative protein target(s) responsible for the observed activity. The second example describes a focused library approach that relied on tandem multicomponent reaction methodologies to afford a series of modulators of the heat shock protein 70 (Hsp70) molecular chaperone. The synthesis of libraries based on the structure of MAL3-101 generated a collection of chemotypes, each modulating Hsp70 function, but exhibiting divergent pharmacological activities. For example, probes that compromise the replication of a disease-associated polyomavirus were identified. These projects highlight the importance of chemical methodology development as a source of small-molecule probes and as a drug discovery starting point.
Transcriptome-wide studies of Merkel cell carcinoma and validation of intratumoral CD8+ lymphocyte invasion as an independent predictor of survival.
Paulson KG, Iyer JG, Tegeder AR, Thibodeau R, Schelter J, Koba S, Schrama D, Simonson WT, Lemos BD, Byrd DR, Koelle DM, Galloway DA, Leonard JH, Madeleine MM, Argenyi AB, Disis ML, Becker JC, Cleary MA, Nghiem P.
J Clin Oncol. 2011 Apr 20;29(12):1539-46.
PMID: 21422430
Abstract and Highlights
- PURPOSE: Merkel cell carcinoma (MCC) is a polyomavirus-associated skin cancer that is frequently lethal and lacks established prognostic biomarkers. This study sought to identify biomarkers that improve prognostic accuracy and provide insight into MCC biology.
- PATIENTS AND METHODS: Gene expression profiles of 35 MCC tumors were clustered based on prognosis. The cluster of genes overexpressed in good-prognosis tumors was tested for biologic process enrichment. Relevant mRNA expression differences were confirmed by quantitative polymerase chain reaction and immunohistochemistry. An independent set of 146 nonoverlapping MCC tumors (median follow-up, 25 months among 116 living patients) was employed for biomarker validation. Univariate and multivariate Cox regression analyses were performed.
- RESULTS: Immune response gene signatures were prominent in patients with good prognoses. In particular, genes associated with cytotoxic CD8+ lymphocytes were overexpressed in tumors from patients with favorable prognoses. In the independent validation set, cases with robust intratumoral CD8+ lymphocyte infiltration had improved outcomes (100% MCC-specific survival, n = 26) compared with instances characterized by sparse infiltration (60% survival, n = 120). Only stage and intratumoral CD8 infiltration (but not age, sex, or CD8+ lymphocytes localized to the tumor-stroma interface) were significant in both univariate and multivariate Cox regression analyses. Notably, traditional histologic identification of tumor-infiltrating lymphocytes was not a significant independent predictor of survival.
- CONCLUSION: Intratumoral CD8+ lymphocyte infiltration can be readily assessed on paraffin-embedded tissue, is independently associated with improved MCC-specific survival, and therefore, may provide prognostic information that enhances established MCC staging protocols.
Merkel cell carcinoma associated with HIV: review of 14 patients.
Izikson L, Nornhold E, Iyer JG, Nghiem P, Zeitouni NC.
AIDS. 2011 Jan 2;25(1):119-21.
PMID: 21119325
2010
Pathologic nodal evaluation improves prognostic accuracy in Merkel cell carcinoma: Analysis of 5,823 cases as the basis of the first consensus staging system for this cancer.
Lemos B, Storer B, Iyer J, Phillips JL, Bichakjian CK, Fang LC, Johnson TM, Liegeois-Kwon NJ, Otley CC, Paulson KG, Ross MI, Yu SS, Zeitouni NC, Byrd DR, Sondak VK, Gershenwald JE, Sober AJ, Nghiem P.
J Am Acad Dermatol. 2010 Nov;63(5):751-61.
PMID: 20646783
Abstract and Highlights
- BACKGROUND: The management of Merkel cell carcinoma (MCC) has been complicated by a lack of detailed prognostic data and by the presence of conflicting staging systems.
- OBJECTIVE: We sought to determine the prognostic significance of tumor size, clinical versus pathologic nodal evaluation, and extent of disease at presentation and thereby derive the first consensus staging/prognostic system for MCC.
- METHODS: A total of 5823 prospectively enrolled MCC cases from the National Cancer Data Base had follow-up data (median 64 months) and were used for prognostic analyses.
- RESULTS: At 5 years, overall survival was 40% and relative survival (compared with age- and sex-matched population data) was 54%. Among all MCC cases, 66% presented with local, 27% with nodal, and 7% with distant metastatic disease. For cases presenting with local disease only, smaller tumor size was associated with better survival (stage I, ≤2 cm, 66% relative survival at 5 years; stage II, >2 cm, 51%; P < .0001). Patients with clinically local-only disease and pathologically proven negative nodes had better outcome (76% at 5 years) than those who only underwent clinical nodal evaluation (59%, P < .0001).
- LIMITATIONS: The National Cancer Data Base does not capture disease-specific survival. Overall survival for patients with MCC was therefore used to calculate relative survival based on matched population data.
- CONCLUSION: Although the majority (68%) of patients with MCC in this nationwide cohort did not undergo pathologic nodal evaluation, this procedure may be indicated in many cases as it improves prognostic accuracy and has important treatment implications for those found to have microscopic nodal involvement.
Antibodies to Merkel cell polyomavirus T-antigen oncoproteins reflect Merkel cell carcinoma tumor burden.
Paulson KG, Carter JJ, Johnson LG, Cahill KW, Iyer JG, Schrama D, Becker JC, Madeleine MM, Nghiem P, Galloway DA.
Cancer Res. 2010 Nov 1;70(21):8388-97.
PMID: 20959478
Abstract and Highlights
- Merkel cell polyomavirus (MCPyV) is a common infectious agent that is likely involved in the etiology of most Merkel cell carcinomas (MCC). Serum antibodies recognizing the MCPyV capsid protein VP1 are detectable at high titer in nearly all MCC patients and remain stable over time. Although antibodies to the viral capsid indicate prior MCPyV infection, they provide limited clinical insight into MCC because they are also detected in more than half of the general population. We investigated whether antibodies recognizing MCPyV large and small tumor-associated antigens (T-Ag) would be more specifically associated with MCC. Among 530 population control subjects, these antibodies were present in only 0.9% and were of low titer. In contrast, among 205 MCC cases, 40.5% had serum IgG antibodies that recognize a portion of T-Ag shared between small and large T-Ags. Among cases, titers of T-Ag antibodies fell rapidly (∼8-fold per year) in patients whose cancer did not recur, whereas they rose rapidly in those with progressive disease. Importantly, in several patients who developed metastases, the rise in T-Ag titer preceded clinical detection of disease spread. These results suggest that antibodies recognizing T-Ag are relatively specifically associated with MCC, do not effectively protect against disease progression, and may serve as a clinically useful indicator of disease status.
Basal cell and squamous cell skin cancers.
Miller SJ, Alam M, Andersen J, Berg D, Bichakjian CK, Bowen G, Cheney RT, Glass LF, Grekin RC, Kessinger A, Lee NY, Liegeois N, Lydiatt DD, Michalski J, Morrison WH, Nehal KS, Nelson KC, Nghiem P, Olencki T, Perlis CS, Rosenberg EW, Shaha AR, Urist MM, Wang LC, Zic JA.
J Natl Compr Canc Netw. 2010 Aug;8(8):836-64.
PMID: 20870631
Radiation monotherapy as regional treatment for node-positive Merkel cell carcinoma.
Fang LC, Lemos B, Douglas J, Iyer J, Nghiem P.
Cancer. 2010 Apr 1;116(7):1783-90. doi: 10.1002/cncr.24919.
PMID: 20162707
Abstract and Highlights
- BACKGROUND: Merkel cell carcinoma (MCC) is an aggressive cutaneous malignancy with a high risk of lymph node involvement. To the authors’ knowledge, few data have been published to date regarding the optimal regional therapy for lymph node-positive patients. This cohort study was performed to analyze the outcomes of patients with lymph node-positive MCC treated with lymph node irradiation as definitive therapy compared with completion lymphadenectomy (CLND).
- METHODS: Fifty patients with lymph node involvement of MCC at presentation and adequate follow-up data were included in this analysis. Forty-three of these patients were enrolled and followed prospectively. Twenty-six patients presented with microscopic lymph node disease, and 24 patients presented with palpable lymph node involvement.
- RESULTS: Regional control for patients with microscopically involved lymph nodes was 100% regardless of treatment modality-definitive lymph node irradiation (n = 19) or CLND +/- radiotherapy (n = 7) with median follow-up of 18 months. Patients with clinically positive lymph nodes had 2-year regional recurrence-free survival rate of 78% and 73% in the definitive lymph node irradiation (n = 9) and CLND +/- radiotherapy (n = 15) groups, respectively (P = .8) with a median follow-up of 16 months.
- CONCLUSIONS: To the best of the authors’ knowledge, the current study is the largest series published to date of radiation monotherapy as regional treatment for lymph node-positive MCC. Lymph node irradiation alone to positive regional lymph nodes was found to confer an excellent regional control rate that was comparable to CLND for both microscopic and palpable lymph node disease. There was no difference noted with regard to overall survival. Given their similar efficacy, the choice between these lymph node therapies may be based on the clinical scenario and anticipated side effect profiles. Cancer 2010. (c) 2010 American Cancer Society.
Protocol for the examination of specimens from patients with Merkel cell carcinoma of the skin.
Rao P, Balzer BL, Lemos BD, Liegeois NJ, McNiff JM, Nghiem P, Prieto VG, Smith MT, Smoller BR, Wick MR, Frishberg DP.
Arch Pathol Lab Med. 2010 Mar;134(3):341-4.
PMID: 20196661
Clinical recognition, diagnosis, and staging of Merkel cell carcinoma, and the role of the multidisciplinary management team.
Sarnaik AA, Lien MH, Nghiem P, Bichakjian CK.
Curr Probl Cancer. 2010 Jan-Feb;34(1):38-46.
PMID: 20371073
2009
Toward better management of Merkel cell carcinoma using a consensus staging system, new diagnostic codes and a recently discovered virus.
Iyer JG, Koba S, Nghiem P.
Actas Dermosifiliogr. 2009 Dec;100 Suppl 2:49-54.
PMID: 20096162
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a neuroendocrine skin cancer with a higher propensity for recurrence and metastasis than melanoma or squamous cell carcinoma. Despite aggressive behavior and the tripling of its reported incidence in the past 20 years, there is extensive confusion about how MCC should be managed. Here we address two issues that have impeded optimal MCC management: lack of a consensus staging system and lack of unique diagnostic codes for MCC. Five conflicting systems currently used to stage MCC will be replaced by one system in 2010 that will diminish confusion about prognosis and management among physicians and patients. The diagnostic bundling of MCC with numerous less aggressive skin cancers leads to care refusals by insurance and an inability to track MCC care costs. Worldwide adoption in 2009 of specific diagnostic codes for MCC will also improve understanding and management of this often-lethal skin cancer.
Association of Merkel Cell Polyomavirus–Specific Antibodies With Merkel Cell Carcinoma
Carter JJ, Paulson KG, Wipf GC, Miranda D, Madeleine MM, Johnson LG, Lemos BD, Lee S, Warcola AH, Iyer JG, Nghiem P, Galloway D.
J Natl Cancer Inst. 2009 Nov 4;101(21):1510-22.
PMID: 19776382
Abstract and Highlights
- BACKGROUND: Merkel cell polyomavirus (MCPyV) has been detected in approximately 75% of patients with the rare skin cancer Merkel cell carcinoma. We investigated the prevalence of antibodies against MCPyV in the general population and the association between these antibodies and Merkel cell carcinoma.
- METHODS: Multiplex antibody-binding assays were used to assess levels of antibodies against polyomaviruses in plasma. MCPyV VP1 antibody levels were determined in plasma from 41 patients with Merkel cell carcinoma and 76 matched control subjects. MCPyV DNA was detected in tumor tissue specimens by quantitative polymerase chain reaction. Seroprevalence of polyomavirus-specific antibodies was determined in 451 control subjects. MCPyV strain-specific antibody recognition was investigated by replacing coding sequences from MCPyV strain 350 with those from MCPyV strain w162.
- RESULTS: We found that 36 (88%) of 41 patients with Merkel cell carcinoma carried antibodies against VP1 from MCPyV w162 compared with 40 (53%) of the 76 control subjects (odds ratio adjusted for age and sex = 6.6, 95% confidence interval [CI] = 2.3 to 18.8). MCPyV DNA was detectable in 24 (77%) of the 31 Merkel cell carcinoma tumors available, with 22 (92%) of these 24 patients also carrying antibodies against MCPyV. Among 451 control subjects from the general population, prevalence of antibodies against human polyomaviruses was 92% (95% CI = 89% to 94%) for BK virus, 45% (95% CI = 40% to 50%) for JC virus, 98% (95% CI = 96% to 99%) for WU polyomavirus, 90% (95% CI = 87% to 93%) for KI polyomavirus, and 59% (95% CI = 55% to 64%) for MCPyV. Few case patients had reactivity against MCPyV strain 350; however, indistinguishable reactivities were found with VP1 from strain 350 carrying a double mutation (residues 288 and 316) and VP1 from strain w162.
- CONCLUSION: Infection with MCPyV is common in the general population. MCPyV, but not other human polyomaviruses, appears to be associated with Merkel cell carcinoma.
ATR-Chk1 pathway inhibition promotes apoptosis after UV treatment in primary human keratinocytes: potential basis for the UV protective effects of caffeine.
Heffernan TP, Kawasumi M, Blasina A, Anderes K, Conney AH, Nghiem P.
J Invest Dermatol. 2009 Jul;129(7):1805-15.
PMID: 19242509
Abstract and Highlights
- New approaches to prevent and reverse UV damage are needed to combat rising sunlight-induced skin cancer rates. Mouse studies have shown that oral or topical caffeine promotes elimination of UV-damaged keratinocytes through apoptosis and markedly inhibits subsequent skin cancer development. This potentially important therapeutic effect has not been studied in human skin cells. Here, we use primary human keratinocytes to examine which of several caffeine effects mediates this process. In these cells, caffeine more than doubled apoptosis after 75 mJ cm(-2) of ultraviolet light B (UVB). Selectively targeting two of caffeine’s known effects did not alter UVB-induced apoptosis: inhibition of ataxia-telangiectasia mutated and augmentation of cyclic AMP levels. In contrast, siRNA against ataxia-telangiectasia and Rad3-related (ATR) doubled apoptosis after UV through a p53-independent mechanism. Caffeine did not further augment apoptosis after UVB in cells in which ATR had been specifically depleted, suggesting that a key target of caffeine in this effect is ATR. Inhibition of a central ATR target, checkpoint kinase 1 (Chk1), through siRNA or a new and highly specific inhibitor (PF610666) also augmented UVB-induced apoptosis. These data suggest that a relevant target of caffeine is the ATR-Chk1 pathway and that inhibiting ATR or Chk1 might have promise in preventing or reversing UV damage.
Array-CGH Reveals Recurrent Genomic Changes in Merkel Cell Carcinoma Including Amplification of L-Myc.
Paulson KG, Lemos BD, Feng B, Jaimes N, Peñas PF, Bi X, Maher E, Cohen L, Leonard JH, Granter SR, Chin L, Nghiem P.
J Invest Dermatol. 2009 Jun;129(6):1547-55.
PMID: 19020549
Abstract and Highlights
- Merkel cell carcinoma (MCC) is an aggressive neuroendocrine skin cancer with poorly characterized genetics. We performed high resolution comparative genomic hybridization on 25 MCC specimens using a high-density oligonucleotide microarray. Tumors frequently carried extra copies of chromosomes 1, 3q, 5p, and 6 and lost chromosomes 3p, 4, 5q, 7, 10, and 13. MCC tumors with less genomic aberration were associated with improved survival (P=0.04). Tumors from 13 of 22 MCC patients had detectable Merkel cell polyomavirus DNA, and these tumors had fewer genomic deletions. Three regions of genomic alteration were of particular interest: a deletion of 5q12-21 occurred in 26% of tumors, a deletion of 13q14-21 was recurrent in 26% of tumors and contains the well-characterized tumor suppressor RB1, and a previously unreported focal amplification at 1p34 was present in 39% of tumors and centers on L-Myc (MYCL1). L-Myc is related to the c-Myc proto-oncogene, has transforming activity, and is amplified in the closely related small cell lung cancer. Normal skin showed no L-Myc expression, whereas 4/4 MCC specimens tested expressed L-Myc RNA in relative proportion to the DNA copy number gain. These findings suggest several genes that may contribute to MCC pathogenesis, most notably L-Myc.
Merkel Cell Carcinoma
Miller SJ, Alam M, Andersen J, Berg D, Bichakjian CK, Bowen G, Cheney RT, Glass LF, Grekin RC, Hallahan DE, Kessinger A, Lee NY, Liegeois N, Lydiatt DD, Michalski J, Morrison WH, Nehal KS, Nelson KC, Nghiem P, Olencki T, Oseroff AR, Perlis CS, Rosenberg EW, Shaha AR, Urist MM, Wang LC.
J Natl Compr Canc Netw. 2009 Mar;7(3):322-32.
PMID: 19401064
Merkel cell polyomavirus is not detected in prostate cancers, surrounding stroma, or benign prostate controls.
Bluemn EG, Paulson KG, Higgins EE, Sun Y, Nghiem P, Nelson PS.
J Clin Virol. 2009 Feb;44(2):164-6.
PMID: 19129009
Abstract and Highlights
- BACKGROUND: Merkel cell polyomavirus (MCV or MCPyV) is a recently discovered human polyomavirus that is implicated in the pathogenesis of Merkel cell carcinoma (MCC). Although the transmission route for MCV is not yet known, other polyomaviruses, such as BKV, cause non-malignant pathology in the urinary tract. Like MCC, prostate cancer predominantly affects the elderly. Furthermore, prostate cancers and premalignant precursors exhibit chronic inflammation, which suggests a possible infectious involvement. We therefore examined whether MCV might participate in the pathogenesis of prostate cancer.
- OBJECTIVE: To determine the presence of MCV RNA in prostate cancer and surrounding stroma or normal prostate tissue.
- STUDY DESIGN: RNA was extracted from 28 patient-matched cancerous and 28 benign prostate epithelial samples, and six additional cancer-adjacent stromal samples. All tissues were laser-capture micro-dissected. DNA and RNA from a sequence-verified MCV-containing MCC tumor served as a positive control. Quantitative reverse-transcription PCR was used to assess the presence or absence of MCV T antigen transcript.
- RESULTS: No MCV T antigen was detected in prostate carcinomas, patient-matched benign samples, or tumor-adjacent stroma, with appropriate sensitivity of the assay demonstrated by an MCC tumor.
- CONCLUSIONS: MCV infection appears unlikely to be a significant factor in prostate carcinogenesis and there is no evidence of the prostate serving as a reservoir for MCV.
Merkel Cell Polyomavirus Is More Frequently Present in North American than Australian Merkel Cell Carcinoma Tumors.
Garneski KM, Warcola AH, Feng Q, Kiviat NB, Leonard JH, Nghiem P.
J Invest Dermatol. 2009 Jan;129(1):246-8. doi: 10.1038/jid.2008.229. Epub 2008 Jul 2
PMID: 18650846
2008
Case 19-2008: Merkel-cell carcinoma.
Lemos BD, Yu SS, Nghiem P.
N Engl J Med. 2008 Oct 9;359(15):1629-30; author reply 1630-1.
PMID: 18843131
Abstract and Highlights
- Comment on: Case records of the Massachusetts General Hospital. Case 19-2008. A 63-year-old HIV-positive man with cutaneous Merkel-cell carcinoma.
Does a new polyomavirus contribute to Merkel cell carcinoma?
Garneski KM1, DeCaprio JA, Nghiem P.
Genome Biol. 2008;9(6):228.
PMID: 18598371
Abstract and Highlights
- A new technique designed to hunt for non-human transcripts has identified a novel SV40-like virus present in the majority of Merkel cell carcinomas. Here we examine what it will take to determine whether or not this virus contributes to carcinogenesis.
Effect of caffeine on the ATR/Chk1 pathway in the epidermis of UVB-irradiated mice.
Lu YP, Lou YR, Pen QY, Xie JG, Nghiem P, Conney AH.
Cancer Res. 2008 Apr 1;68(7):2523-9.
PMID: 18381462
Abstract and Highlights
- Administration of caffeine was shown in earlier studies to enhance UVB-induced apoptosis and inhibit UVB-induced carcinogenesis in hairless SKH-1 mice. Here, we describe a potential mechanism for these in vivo effects. A single irradiation of mouse skin with UVB activated the ataxia-telangiectasia mutated- and Rad3-related (ATR) pathway, causing a severalfold increase in keratinocytes with phospho-Chk1 (Ser(345)) and a marked decrease in mitotic keratinocytes with cyclin B1 compared with baseline. When given in the drinking water for 1 to 2 weeks before UVB, caffeine (0.4 mg/mL) markedly inhibited the UVB-induced phosphorylation of Chk1 on Ser(345) and caused premature expression of cyclin B1 in the epidermis. Normal keratinocytes had delayed mitotic entry for >10 h following UVB. Caffeine administration reduced this mitotic delay to only 4 h and caused markedly increased apoptosis by 6 to 10 h after UVB. p53 knockout mice were used to determine the role of p53 in these processes. Irradiation with UVB markedly decreased the number of mitotic keratinocytes with cyclin B1 in p53 knockout mice, and topical caffeine immediately after UVB abrogated this response and increased UVB-induced apoptosis severalfold. These effects of caffeine in knockout mice were substantially greater than in wild-type mice. The ability of caffeine to promote the deletion of p53(-/-) keratinocytes may be relevant to its inhibitory effect on UVB-induced skin cancer. Our studies indicate that administration of caffeine enhances the removal of DNA-damaged cells by inhibiting the ATR-mediated phosphorylation of Chk1 and prematurely increasing the number of cyclin B1-containing cells that undergo lethal mitosis.
Clinical characteristics of Merkel cell carcinoma at diagnosis in 195 patients: the “AEIOU” Features.
Heath M, Jaimes N, Lemos B, Mostaghimi A, Wang L, Penas P, Nghiem, P.
J Am Acad Dermatol. 2008 Mar;58(3):375-81
2007
Merkel cell carcinoma: more deaths but still no pathway to blame.
Lemos B, Nghiem P.
J Invest Dermatol. 2007 Sep;127(9):2100-3.
PMID: 17700621
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a neuroendocrine skin cancer with a rising incidence (1500 U.S. cases per year) that now exceeds that of cutaneous T-cell lymphoma and a mortality (33%) exceeding that of melanoma. Despite this impact, little is known about its biology. Recent studies have shown that Ras/MAP kinase activity is absent and possibly detrimental to this cancer. This makes MCC distinct from other UV–induced skin cancers and highlights the question of what drives this malignancy.
Merkel cell carcinoma adjuvant therapy: current data support radiation but not chemotherapy.
Garneski KM, Nghiem P.
J Am Acad Dermatol. 2007 Jul;57(1):166-9. Epub 2007 May 7.
PMID: 17482714
Abstract and Highlights
- Merkel cell carcinoma (MCC) is a skin cancer with 30% mortality and an incidence that has tripled in the past 15 years. There is agreement that surgical excision with negative margins is an appropriate therapeutic first step and that sentinel lymph node biopsy is a powerful prognostic indicator. After excision of detectable cancer, optimal adjuvant therapy is not well established. A role for adjuvant radiotherapy is increasingly supported by observational data. These data suggest that a regimen of surgery plus adjuvant radiotherapy is associated with both a lower loco-regional recurrence rate and longer overall survival when compared with surgery alone. In contrast, a role for adjuvant chemotherapy is not well supported. The rationale for chemotherapy in this disease is based on small-cell lung cancer, a more common neuroendocrine tumor for which chemotherapy is the primary treatment modality. Several issues call into question the routine use of adjuvant chemotherapy in MCC: lack of evidence for improved survival; the associated morbidity and mortality; important differences between small-cell lung cancer and MCC; and rapid development of resistance to chemotherapy. Importantly, chemotherapy suppresses immune function that plays an unusually large role in defending the host from the development and progression of MCC. Taken together, these arguments suggest that adjuvant radiation may be indicated for many MCC patients while adjuvant chemotherapy should largely be restricted to clinical trials.
Chemical genetics: elucidating biological systems with small-molecule compounds.
Kawasumi M, Nghiem P.
J Invest Dermatol. 2007 Jul;127(7):1577-84.
PMID: 17568801
Abstract and Highlights
- Chemical genetics employs diverse small-molecule compounds to elucidate biological processes in a manner analogous to the mutagenesis strategies at the core of classical genetics. Screening small-molecule libraries for compounds that induce a phenotype of interest represents the forward chemical genetic approach, whereas the reverse approach involves small molecules targeting a single protein. Here, we review key differences between the goals for small-molecule screening in industry versus academia, recent developments in high-throughput screening, and publicly available resources of compound collections, screening facilities, and databases. A particularly exciting outcome of a chemical genetic screen is the discovery of a previously unknown role for a protein in a pathway together with compounds that affect the function of that protein. In illustrative cases, such discoveries have led to progress toward therapeutic development and more commonly have increased the size of the small molecule “toolbox” available to the research community for the study of biological processes.
Merkel cell carcinoma: if no breslow, then what?
Heath ML, Nghiem P.
J Surg Oncol. 2007 Jun 15;95(8):614-5.
PMID: 17221860
Abstract and Highlights
- Comment on: Prognostic value of tumor thickness in patients with Merkel cell carcinoma
Protection from photodamage by topical application of caffeine after ultraviolet irradiation.
Koo SW, Hirakawa S, Fujii S, Kawasumi M, Nghiem P.
Br J Dermatol. 2007 May;156(5):957-64. Epub 2007 Mar 28.
PMID: 17388926
Abstract and Highlights
- BACKGROUND: Characterization of mechanisms that can reverse residual damage from prior skin exposure to ultraviolet (UV) would be of considerable biological and therapeutic interest. Topical caffeine application to mouse skin that had previously been treated with UV has been shown to inhibit the subsequent development of squamous cell carcinomas.
- OBJECTIVES: We used an established mouse photodamage model to investigate other possible effects of topical caffeine application after UV.
- METHODS: SKH-1 hairless mice were treated with ultraviolet B (UVB) followed immediately by topical application of caffeine or vehicle three times weekly for 11 weeks.
- RESULTS: Caffeine applied topically after UV treatment resulted in a significant decrease in UV-induced skin roughness/transverse rhytides as assessed by treatment-blinded examiners. Histologically, topical caffeine application after a single dose of UVB more than doubled the number of apoptotic keratinocytes as evaluated by sunburn cell formation, caspase 3 cleavage and terminal deoxynucleotidyl transferase-mediated dUTP-biotin nick-end labelling (TUNEL) staining. A trend towards decreased solar elastosis was noted in the caffeine-treated group although this was not statistically significant. Other histological parameters including epidermal hyperplasia, solar elastosis and angiogenesis were increased in mice treated with UV but topical application of caffeine did not alter these particular UV effects.
- CONCLUSIONS: These findings support the concept that topical application of caffeine to mouse skin after UV irradiation promotes the deletion of DNA-damaged keratinocytes and may partially diminish photodamage as well as photocarcinogenesis.
Dermatofibrosarcoma Protuberans Guidelines
Miller SJ, Alam M, Andersen J, Berg D, Bichakjian CK, Bowen G, Cheney RT, Glass F, Grekin RC, Grichnik JM, Kessinger A, Lee NY, Lessin S, Lydiatt DD, Margolis LW, Michalski J, Nehal KS, Nghiem P, Oseroff AR, Rosenberg EW, Shaha AR, Siegle RJ, Urist MM
J Natl Compr Canc Netw. 2007 May;5(5):550-5.
PMID: 17509257
Abstract and Highlights
- Dermatofibrosarcoma protuberans (DFSP) is an uncommon, low-grade sarcoma of fibroblast origin with an incidence rate of 0.8 cases per million persons each year. Although it rarely metastasizes, initial misdiagnosis, prolonged time to accurate diagnosis, and large tumor size at diagnosis are common. These updated 2007 guidelines include changes in recommendations for considering radiation therapy, as well as those regarding surgical margins in some patients.
The Protective Role of a Small GTPase RhoE against UVB-induced DNA Damage in Keratinocytes.
Boswell SA, Ongusaha PP, Nghiem P, Lee SW.
J Biol Chem. 2007 Feb 16;282(7):4850-8. Epub 2006 Dec 14.
PMID: 17170105
Abstract and Highlights
- RhoE, a p53 target gene, was identified as a critical factor for the survival of human keratinocytes in response to UVB. The Rho family of GTPases regulates many aspects of cellular behavior through alterations to the actin cytoskeleton, acting as molecular switches cycling between the active, GTP-bound and the inactive, GDP-bound conformations. Unlike typical Rho family proteins, RhoE (also known as Rnd3) is GTPase-deficient and thus expected to be constitutively active. In this study, we investigated the response of cultured human keratinocyte cells to UVB irradiation. RhoE protein levels increase upon exposure to UVB, and ablation of RhoE induction through small interfering RNA resulted in a significant increase in apoptosis and a reduction in the levels of the pro-survival targets p21, Cox-2, and cyclin D1, as well as an increase of reactive oxygen species levels when compared with control cells. These data indicate that RhoE is a pro-survival factor acting upstream of p38, JNK, p21, and cyclin D1. HaCat cells expressing small interfering RNA to p53 indicate that RhoE functions independently of its known associates, p53 and Rho-associated kinase I (ROCK I). Targeted expression of RhoE in epidermis using skin-specific transgenic mouse model resulted in a significant reduction in the number of apoptotic cells following UVB irradiation. Thus, RhoE induction counteracts UVB-induced apoptosis and may serve as a novel target for the prevention of UVB-induced photodamage regardless of p53 status.
2006
Sentinel lymph node biopsy for evaluation and treatment of patients with Merkel Cell Carcinoma.
Gupta SG, Wang LC, Penas PF, Gellenthin M, Lee SJ, Nghiem P.
Arch Dermatol. 2006 Jun;142(6):685-90.
PMID: 16785370
Abstract and Highlights
- OBJECTIVE: To determine the diagnostic accuracy and usefulness of sentinel lymph node biopsy (SLNB) and computed tomographic scans in the initial evaluation and treatment of patients with Merkel cell carcinoma (MCC).
- DESIGN: Single-institution case series and literature-based case-level meta-analysis.
- SETTING: Academic cutaneous oncology clinic.Patients Sixty-one adults with biopsy-proven MCC (30 who had undergone SLNB) plus 92 cases from the literature of patients who had undergone SLNB.
- MAIN OUTCOME MEASURES: Relapse-free survival.
- RESULTS: In 122 patients with no nodal disease found by physical examination, SLNB findings revealed nodal involvement in 39 cases (32%). At 3 years, the recurrence rate for those with a positive SLNB was 3 times (60%) higher than for those with a negative SLNB (20%; P = .03). Patients with a positive SLNB who received adjuvant nodal therapy had a relapse-free survival rate of 51% at 3 years (n = 26) compared with 0% for patients who did not receive nodal therapy (n = 3; P < .01). In contrast, among patients with a negative SLNB there was no significant difference in 3-year relapse-free survival rates for those who did (90%; n = 24) or did not (70%; n = 19; P = .26) receive adjuvant nodal therapy. Using SLNB plus clinical follow-up as a gold standard, computed tomographic scans had low sensitivity (20%) for detecting MCC that had spread to the lymph node basin and low specificity for distant disease (only 4 of 21 “positive” scans were confirmed during 6 months of follow-up).
- CONCLUSIONS: Sentinel lymph node biopsy detects MCC spread in one third of patients whose tumors would have otherwise been clinically and radiologically understaged and who may not have received treatment to the involved node bed. There was a significant benefit of adjuvant nodal therapy, but only when the SLNB was positive. Thus, SLNB is important for both prognosis and therapy and should be performed routinely for patients with MCC. In contrast, computed tomographic scans have poor sensitivity in detecting nodal disease as well as poor specificity in detecting distant disease.
A robust small-molecule microarray platform for screening cell lysates.
Bradner JE, McPherson OM, Mazitschek R, Barnes-Seeman D, Shen JP, Dhaliwal J, Stevenson KE, Duffner JL, Park SB, Neuberg DS, Nghiem P, Schreiber SL, Koehler AN.
Chem Biol. 2006 May;13(5):493-504.
PMID: 16720270
Abstract and Highlights
- Herein we report the expanded functional group compatibility of small-molecule microarrays to include immobilization of primary alcohols, secondary alcohols, phenols, carboxylic acids, hydroxamic acids, thiols, and amines on a single slide surface. Small-molecule “diversity microarrays” containing nearly 10,000 known bioactive small molecules, natural products, and small molecules originating from several diversity-oriented syntheses were produced by using an isocyanate-mediated covalent capture strategy. Selected printed bioactive compounds were detected with antibodies against compounds of interest. The new surface of the diversity microarrays is highly compatible with approaches involving cellular lysates. This feature has enabled a robust, optimized screening methodology using cellular lysates, allowing the detection of specific interactions with a broad range of binding affinity by using epitope-tagged or chimeric fluorescent proteins without prior purification. We believe that this expanded research capability has considerable promise in biology and medicine.
Role of skin biopsy to confirm suspected acute graft vs. host disease: results of decision analysis.
Firoz B, Lee S, Nghiem, P, Qureshi A.
Arch Dermatol. 2006 Feb;142(2):175-82.
PMID: 16490845
Abstract and Highlights
- Objective: To estimate the value of skin biopsy in the evaluation of suspected acute cutaneous graft-vs-host disease (GVHD) after allogeneic stem cell transplantation.
- Design: Decision analysis using parameters specified by expert opinion for skin biopsy characteristics, prevalence of acute GVHD, and value of potential outcomes. One-, 2-, and 3-way sensitivity analyses were performed.
- Setting Major stem cell transplantation centers in the United States.
- Patients Hypothetical cohort of patients with suspected acute cutaneous GVHD after stem cell transplantation.
- Interventions: The following 3 interventions were compared: treat immediately for GVHD without performing a skin biopsy, perform a skin biopsy and treat immediately but stop treatment if skin biopsy specimen findings are inconsistent with GVHD, and perform a skin biopsy and await results of the skin biopsy specimen before treating.
- Main Outcome Measures: Number of patients appropriately and inappropriately treated with each intervention, consistency of physician-reported behavior, individualized decision analyses, and preferred intervention based on the aggregate estimates of res;pondents.
- Results: The decision to treat immediately for GVHD without performing a skin biopsy yielded the best clinical outcome for the specified clinical setting and under the parameters specified by expert opinion. One-way sensitivity analyses showed that these conclusions are robust if the prevalence of acute cutaneous GVHD in stem cell recipients with rash is greater than 50%, if the sensitivity of skin biopsy specimen is less than 0.8, and the specificity of skin biopsy specimen is less than 0.9. Only 25% of physicians interviewed chose an intervention consistent with their estimates of prevalence, test characteristics, and outcome evaluations, indicating an opportunity to improve management of this important clinical condition.
- Conclusions: This decision analysis modeling technique predicts that in patient populations in which the prevalence of GVHD is 30% or greater (typical for allogeneic stem cell transplantation), the best outcomes were obtained with treatment for GVHD and no skin biopsy. In populations with prevalence of GVHD of 30% or less, obtaining a skin biopsy specimen to guide treatment was predicted to provide the best patient outcomes.
- Acute graft-vs-host disease (GVHD) in allogeneic stem cell transplantation (SCT) is a complex immunologic phenomenon involving donor T cells, cytokines, and host tissue reactions. Graft-vs-host disease is a frequent complication of SCT. Acute GVHD manifests in the first 3 months after transplantation, and the main target organs include the skin, the liver, and the gastrointestinal tract. Clinical features of acute cutaneous GVHD include a disseminated exanthem characterized by acral erythema and often a scarlatiniform eruption that may progress to erythroderma.1 Clinically significant acute GVHD is estimated to occur in 6% to 90% of graft recipients, depending on patient age, HLA type, and prevention protocols used.2 A clinical staging system (grades 0 [best] to IV [worse]) based on degree of organ involvement has been used as an important prognostic indicator. The diagnosis of acute GVHD can have profound implications on prognosis; approximately 90% of patients with no or minimal (grade I) acute GVHD survive to day 100 compared with 60% of patients with grades II or III disease and 0% to 20% of patients with grade IV disease.3 Staging and grading criteria for acute GVHD used in this study are summarized in Table 1.
- Initially, the diagnosis of acute GVHD involving the skin is difficult to make because the eruption can be morphologically nonspecific, appearing as an erythematous macular rash. Differential diagnosis of an erythematous rash is broad in patients after SCT and includes cutaneous reactions to chemotherapy or radiation therapy, adverse drug reactions, and viral infections. In a patient with a skin eruption, the presence of extracutaneous GVHD is helpful in making the diagnosis and determining the need for therapy. However, hepatic and gastrointestinal tract involvement often are not present because the skin is the most common site of GVHD and frequently is the first organ to demonstrate clinical findings. Further workup usually includes obtaining a skin biopsy specimen.
- Significant controversy involves the use and timing of skin biopsy in the diagnosis of acute cutaneous GVHD in SCT recipients. The value of obtaining a skin biopsy specimen after SCT depends on at least 2 schools of thought about acute GVHD management. Some clinicians assert that cautious use of immunosuppression therapy is warranted because of the high risk for sepsis in patients recovering from SCT. Others maintain that delaying appropriate therapy for GVHD can lead to rapid progression of the disease and that, therefore, immunosuppression therapy should be considered immediately in patients with a skin eruption when the probability of GVHD is high.5 This rationale is supported by the high prevalence of GVHD in patients who have an erythematous eruption involving more than 60% of the body surface area a few days after undergoing SCT.
- Although the sensitivity and specificity of a skin biopsy specimen in suspected acute GVHD has not been established, clinicians continue to obtain skin biopsy specimens when considering the possibility of acute GVHD after SCT. Previous studies have established that certain histologic changes evident in patients with acute GVHD, such as lymphocytic infiltrate at the basement membrane with exocytosis and spongiosis, are pathologically indistinguishable from common differential diagnoses of rash after SCT, including irradiation dermatitis and drug reactions.6,7 Another study demonstrated that in 80% of rush skin biopsy specimens obtained after SCT the findings were interpreted by pathologists as nonspecific and unequivocal, 76% of patients were treated empirically before biopsy specimen results were available, and in only 5.5% of patients was treatment changed based on biopsy specimen results.8 A recent retrospective analysis showed that skin biopsy specimen findings are poorly correlated with the clinical severity of rash suggestive of acute GVHD early after SCT.9 This study found no significant difference between patients with positive biopsy specimen findings and those with negative biopsy specimen findings, either in the clinical severity of acute GVHD or in the likelihood of receiving treatment for GVHD. They found that the decision to treat suspected acute GVHD depended on clinical suspicion, not on biopsy specimen findings, and, therefore, suggested that skin biopsy has a limited role in the management of eruptions in the early period after SCT.
- Inasmuch as the optimal management intervention likely hinges on the pretest probability of acute GVHD, the test characteristics of the skin biopsy specimen to confirm acute GVHD (sensitivity and specificity), and the relative consequences of appropriate and inappropriate treatment, we performed a decision analysis to investigate the interaction between these factors. Decision analysis is a method to aggregate diverse considerations pertinent to a decision so that the best clinical choice can be made in the absence of clear experimental or observational data.10,11 Hence, this approach enables simultaneous consideration of the risks and benefits of skin biopsy after SCT: appropriate treatment of GVHD, missed or delayed treatment of GVHD in patients with negative skin biopsy specimen findings, and inappropriate treatment in patients without GVHD but with positive skin biopsy specimen findings. A traditional decision analysis model would use survival curves, receiver operating characteristic curves, and other evidence-based data. An extensive literature search failed to provide data necessary for the model, including sensitivity and specificity of skin biopsy specimens and occurrence of adverse outcomes. Therefore, this modeling approach used expert opinion to estimate test characteristics of skin biopsy specimens and to provide valuations for the relative benefit-risk ratio of appropriate vs inappropriate treatment of GVHD. Our results should be used to guide further research to better understand the role of skin biopsy after SCT.
2004
HIV-1 Vpr-mediated G2 arrest requires Rad17 and Hus1 and induces nuclear BRCA1 and gamma-H2AX foci formation.
Zimmerman E, Chen J, Blackett J, DeHart J, Murala S, Andersen J, Ardon O, Nghiem P, Planelles V.
Mol Cell Biol. 2004 Nov;24(21):9286-94.
PMID: 15485898
Abstract and Highlights
- Eukaryotic cells have evolved a complex mechanism for sensing DNA damage during genome replication. Activation of this pathway prevents entry into mitosis to allow for either DNA repair or, in the event of irreparable damage, commitment to apoptosis. Under conditions of replication stress, the damage signal is initiated by the ataxia-telangiectasia-mutated and Rad3-related kinase ATR. We recently demonstrated that the human immunodeficiency virus type 1 (HIV-1) gene product viral protein R (Vpr) arrests infected cells in the G(2) phase via the activation of ATR. In the present study, we show that the activation of ATR by Vpr is analogous to activation by certain genotoxic agents, both mechanistically and in its downstream consequences. Specifically, we show a requirement for Rad17 and Hus1 to induce G(2) arrest as well as Vpr-induced phosphorylation of histone 2A variant X (H2AX) and formation of nuclear foci containing H2AX and breast cancer susceptibility protein 1. These results demonstrate that G(2) arrest mediated by the HIV-1 gene product Vpr utilizes the cellular signaling pathway whose physiological function is to recognize replication stress. These findings should contribute to a greater understanding of how HIV-1 manipulates the CD4(+)-lymphocyte cell cycle and apoptosis induction in the progressive CD4(+)-lymphocyte depletion characteristic of HIV-1 pathogenesis.
Tissue eosinophils and the perils of using skin biopsy specimens to distinguish between drug hypersensitivity and cutaneous graft-vs.-host disease.
Marra D, McKee P, Nghiem P.
J Am Acad Dermatol. 2004 Oct;51(4):543-6.
PMID: 15389188
Abstract and Highlights
- Graft-versus-host disease (GvHD) is a frequent and serious complication of bone-marrow transplantation (BMT), and carries a high morbidity and mortality if not promptly recognized and treated. The rash of acute GvHD is often difficult to distinguish clinically from a drug eruption, and skin biopsies are often performed in an attempt to render a diagnosis. Histologically, eosinophils are classically associated with hypersensitivity reactions, and their presence in inflamed tissue is considered suggestive of a drug-induced dermatitis. We present 3 cases of acute exanthema in BMT recipients in whom the presence of eosinophils on skin biopsy specimen led to an initial diagnosis of drug eruption over GvHD. As a result, these patients experienced delays in the institution of definitive immunosuppressive therapy for GvHD. We review the growing literature suggesting that no single or combined histologic feature, including tissue eosinophils, is useful in differentiating GvHD from drug eruptions in BMT recipients. Indeed, in most cases, the cause of a new-onset blanchable erythematous rash in a BMT recipient is most accurately determined by close examination and follow-up of the clinical features without a skin biopsy.
2003
Merkel cell carcinoma treatment with radiation: A good case despite no prospective studies.
Longo I, Nghiem P.
Arch Dermatol. 2003 Dec;139(12):1641-3.
PMID: 14676085
Integration of growth factor and nutrient signaling: Implications for cancer biology.
Shamji S, Nghiem P, Schreiber S.
Mol Cell. 2003 Aug;12(2):271-80.
PMID: 14536067
Abstract and Highlights
- Signaling networks that promote cell growth are frequently dysregulated in cancer. One regulatory network, which converges on effectors such as 4EBP1 and S6K1, leads to growth by promoting protein synthesis. Here, we discuss how this network is regulated by both extracellular signals, such as growth factors, and intracellular signals, such as nutrients. We discuss how mutations amplifying either type of signal can lead to tumor formation. In particular, we focus on the recent discovery that a tumor suppressor complex whose function is lost in tuberous sclerosis patients regulates the nutrient signal carried by the critical signaling protein TOR to the effectors 4EBP1 and S6K1. Finally, we describe how the small molecule rapamycin, which inhibits TOR and thereby the activation of these effectors, could be useful to treat tumors that have become dependent upon this pathway for growth.
Activation of the ATR-mediated DNA Damage Response by the HIV-1 Viral Protein R.
Roshal M, Kim B, Zhu Y, Nghiem P, Planelles V.
J Biol Chem. 2003 Jul 11;278(28):25879-86. Epub 2003 May 8
PMID: 12738771
Abstract and Highlights
- DNA damage is a universal inducer of cell cycle arrest at the G2 phase. Infection by the human immunodeficiency virus type 1 (HIV-1) also blocks cellular proliferation at the G2 phase. The HIV-1 accessory gene vpr encodes a conserved 96-amino acid protein (Vpr) that is necessary and sufficient for the HIV-1-induced block of cellular proliferation. In the present study, we examined a recently identified DNA damage-signaling protein, the ATM- and Rad3-related protein, ATR, for its potential role in the induction of G2 arrest by Vpr. We show that inhibition of ATR by pharmacological inhibitors, by expression of the dominant-negative form of ATR, or by RNA interference inhibits Vpr-induced cell cycle arrest. As with DNA damage, activation of ATR by Vpr results in phosphorylation of Chk1. This study provides conclusive evidence of activation of the ATR-initiated DNA damage-signaling pathway by a viral gene product. These observations are important toward understanding how HIV infection promotes cell cycle disruption, cell death, and ultimately, CD4+ lymphocyte depletion.
2002
ATR Regulates Fragile Site Stability.
Casper A, Nghiem P, Arlt M, Glover T.
Cell. 2002 Dec 13;111(6):779-89.
PMID: 12526805
Abstract and Highlights
- Conditions that partially inhibit DNA replication induce expression of common fragile sites. These sites form gaps and breaks on metaphase chromosomes and are deleted and rearranged in many tumors. Yet, the mechanism of fragile site expression has been elusive. We demonstrate that the replication checkpoint kinase ATR, but not ATM, is critical for maintenance of fragile site stability. ATR deficiency results in fragile site expression with and without addition of replication inhibitors. Thus, we propose that fragile sites are unreplicated chromosomal regions resulting from stalled forks that escape the ATR replication checkpoint. These findings have important implications for understanding both the mechanism of fragile site instability and the consequences of stalled replication in mammalian cells.
ATR Regulates Fragile Site Stability.
Casper A, Nghiem P, Arlt M, Glover T.
Cell. 2002 Dec 13;111(6):779-89.
PMID: 12526805
Abstract and Highlights
- Conditions that partially inhibit DNA replication induce expression of common fragile sites. These sites form gaps and breaks on metaphase chromosomes and are deleted and rearranged in many tumors. Yet, the mechanism of fragile site expression has been elusive. We demonstrate that the replication checkpoint kinase ATR, but not ATM, is critical for maintenance of fragile site stability. ATR deficiency results in fragile site expression with and without addition of replication inhibitors. Thus, we propose that fragile sites are unreplicated chromosomal regions resulting from stalled forks that escape the ATR replication checkpoint. These findings have important implications for understanding both the mechanism of fragile site instability and the consequences of stalled replication in mammalian cells.
2001
Tacrolimus Ointment in the Treatment of Chronic Cutaneous Graft-vs.-Host Disease: A Case Series of 18 Patients.
Choi C, Nghiem P.
Arch Dermatol. 2001 Sep;137(9):1202-6.
PMID: 11559218
Abstract and Highlights
- Objective: To assess the therapeutic efficacy of 0.1% tacrolimus ointment on chronic cutaneous GVHD in patients with symptoms refractory to systemic corticosteroid therapy.
- Results: Tacrolimus ointment effectively treated pruritus and/or erythema in 13 (72%) of 18 patients with chronic GVHD. Responding patients had a rapid effect within several hours to days. Effectiveness was measured by means of patient report, results of physical examination, side-by-side comparisons of tacrolimus vs a vehicle control, and temporal flares of the cutaneous symptoms of the disease in the context of stopping tacrolimus ointment therapy. Because of the progression of GVHD and in 2 cases, loss of drug efficacy, all patients eventually went on to receive more aggressive treatment, including increases in steroid dosage, psoralen–UV-A therapy, and extracorporeal photopheresis.
- Conclusions: This case series suggests that tacrolimus ointment has efficacy in treating the erythema and pruritus of steroid-refractory, chronic cutaneous GVHD in most patients. The rapid response of tacrolimus ointment may provide a useful therapeutic bridge to systemic therapies that have slower onset, such as psoralen–UV-A therapy or extracorporeal photopheresis.”
ATR Inhibition Selectively Sensitizes G1 Checkpoint-Deficient Cells To Lethal Premature Chromatin Condensation.
Nghiem P, Park P, Kim Y, Vaziri C, Schreiber S.
Proc Natl Acad Sci U S A. 2001 Jul 31;98(16):9092-7.
PMID: 11481475
Abstract and Highlights
- Premature chromatin condensation (PCC) is a hallmark of mammalian cells that begin mitosis before completing DNA replication. This lethal event is prevented by a highly conserved checkpoint involving an unknown, caffeine-sensitive mediator. Here, we have examined the possible involvement of the caffeine-sensitive ATM and ATR protein kinases in this checkpoint. We show that caffeine’s ability to inhibit ATR (but not ATM) causes PCC, that ATR (but not ATM) prevents PCC, and that ATR prevents PCC via Chk-1 regulation. Moreover, mimicking cancer cell phenotypes by disrupting normal G(1) checkpoints sensitizes cells to PCC by ATR inhibition plus low-dose DNA damage. Notably, loss of p53 function potently sensitizes cells to PCC caused by ATR inhibition by a small molecule. We present a molecular model for how ATR prevents PCC and suggest that ATR represents an attractive therapeutic target for selectively killing cancer cells by premature chromatin condensation.
2000
Identifying the Missing Link Between UV and p53: The Role of Phosphatidyl Inositol Kinase-Related Kinases.
Nghiem P.
J Am Acad Dermatol. 2000 Oct;43(4):706-7
PMID: 11004635
Abstract and Highlights
- ATR (ataxia telangiectasia and Rad-3-related) is a protein kinase required for survival after DNA damage. A critical role for ATR has been hypothesized to be the regulation of p53 and other cell cycle checkpoints. ATR has been shown to phosphorylate p53 at Ser(15), and this damage-induced phosphorylation is diminished by expression of a catalytically inactive (ATR-kd) mutant. p53 function could not be examined directly in prior studies of ATR, however, because p53 was mutant or because cells expressed the SV40 large T antigen that blocks p53 function. To test the interactions of ATR and p53 directly we generated human U2OS cell lines inducible for either wild-type or kinase-dead ATR that also have an intact p53 pathway. Indeed, ATR-kd expression sensitized these cells to DNA damage and caused a transient decrease in damage-induced serine 15 phosphorylation of p53. However, we found that the effects of ATR-kd expression do not result in blocking the response of p53 to DNA damage. Specifically, prior ATR-kd expression had no effect on DNA damage-induced p53 protein up-regulation, p53-DNA binding, p21 mRNA up-regulation, or G(1) arrest. Instead of promoting survival via p53 regulation, we found that ATR protects cells by delaying the generation of mitotic phosphoproteins and inhibiting premature chromatin condensation after DNA damage or hydroxyurea. Although p53 inhibition (by E6 or MDM2 expression) had little effect on premature chromatin condensation, when combined with ATR-kd expression there was a marked loss of the replication checkpoint. We conclude that ATR and p53 can function independently but that loss of both leads to synergistic disruption of the replication checkpoint
The standard of care for Merkel cell carcinoma should include adjuvant radiation and lymph node surgery.
Herbst A, Haynes HA, Nghiem P.
J Am Acad Dermatol. 2002 Apr;46(4):640-2.
PMID: 11907528
1994
“Topical immunomodulators?”: introducing old friends and a new ally, tacrolimus.
Nghiem P, Ollick T, Gardner P, Schulman H.
Nature. 1994 Sep 22;371(6495):347-50.
PMID: 8090206
Abstract and Highlights
- In the presence of costimulation, Ca2+ influx in T cells leads to activation (transcription of interleukin-2; ref. 2) via calcineurin. In the absence of costimulation, Ca2+ influx results in anergy (interleukin-2 transcriptional block) through an unknown mechanism. Specific attenuation of interleukin-2 transcriptional induction occurs in Jurkat T cells following pretreatment with a Ca2+ ionophore. A > 90% block of inducible interleukin-2 reporter gene activity was initiated by transfection of a constitutively active mutant of multifunctional Ca2+/calmodulin-dependent protein kinase (CaM kinase or CaM kinase II), but not by constitutive mutants of CaM kinase IV, calcineurin or protein kinase C. The block was complete six hours after kinase transfection and showed specificity for interleukin-2; there was no change in beta-actin transcription or in c-fos transcription induced by phorbol myristyl acetate, and a Rous sarcoma virus promoter was stimulated threefold. Multifunctional CaM kinase also attenuated interleukin-2 activation by calcineurin plus phorbol ester. T-cell receptor signalling activates multifunctional CaM kinase. These findings suggest that two Ca2+/calmodulin-responsive enzymes, multifunctional CaM kinase and calcineurin, could mediate the divergent effects of Ca2+ signals in T-lymphocyte regulation.
Limiting Dilution Analysis of Ontogeny of Self- and Allo-Reactive Thymocytes of C57BL/6J Mouse.
Itoh T, Rao A, O'Brien D, Nghiem P, Cantor H.
Cytogenet Cell Genet. 1994;66(2):113-6.
PMID: 2256126
Abstract and Highlights
- Multifunctional calcium/calmodulin-dependent protein kinase (CaM kinase) is an enzyme mediating calcium-dependent signal transduction pathways. CaM kinase exists in a variety of isoforms, each with a distinct tissue-specific expression pattern, that enables the kinase to regulate multiple functions in mammalian systems. Here we report the chromosomal localization of the previously cloned human gamma-CaM kinase gene (CAMKG). By using a mapping panel of human x Chinese hamster somatic cell hybrid lines and fluorescence in situ hybridization, we have assigned human CAMKG to chromosome 10q22. We have partially cloned the murine gamma-CaM kinase gene and mapped it Camkg to mouse chromosome 14 by analyzing a panel of mouse x rodent somatic cell hybrid lines. A recessive gene, asa, implicated in the control of autoimmune response, is located within the predicted region for Camkg.
Localization of the CAMKG Gene Encoding Gamma Isoforms of Multifunctional Calcium/calmodulin-dependent Protein Kinase (CaM Kinase) to Human Chromosome 10 Band q22 and Mouse Chromosome 14.
Li X, Nghiem P, Schulman H, Francke U.
Cytogenet Cell Genet. 1994;66(2):113-6.
PMID: 8287681
Abstract and Highlights
- Multifunctional calcium/calmodulin-dependent protein kinase (CaM kinase) is an enzyme mediating calcium-dependent signal transduction pathways. CaM kinase exists in a variety of isoforms, each with a distinct tissue-specific expression pattern, that enables the kinase to regulate multiple functions in mammalian systems. Here we report the chromosomal localization of the previously cloned human gamma-CaM kinase gene (CAMKG). By using a mapping panel of human x Chinese hamster somatic cell hybrid lines and fluorescence in situ hybridization, we have assigned human CAMKG to chromosome 10q22. We have partially cloned the murine gamma-CaM kinase gene and mapped it Camkg to mouse chromosome 14 by analyzing a panel of mouse x rodent somatic cell hybrid lines. A recessive gene, asa, implicated in the control of autoimmune response, is located within the predicted region for Camkg.
1993
Cloning and Analysis of Two New Isoforms of Multifunctional Calcium/Calmodulin-dependent Protein Kinase Expressed in Multiple Human Tissues.
Nghiem P, Saati S, Martens C, Gardner P, Schulman H.
J Biol Chem. 1993 Mar 15;268(8):5471-9.
PMID: 8449910
Abstract and Highlights
- Multifunctional Ca2+/calmodulin-dependent protein kinase (CaM kinase) is a mediator of calcium signals in diverse signaling pathways. In human lymphocytes and epithelial tissues, CaM kinase activates a chloride channel via a Ca(2+)-dependent pathway which is preserved in cystic fibrosis. To characterize the CaM kinase present in these tissues we have cloned an isoform of this kinase from human T lymphocytes. We show the cDNA structure of two variants of this human CaM kinase, gamma B and gamma C, which are predicted to translate to 518 and 495 amino acids, respectively. Amino acid differences between these isoforms and the rat brain gamma isoform (which we refer to as gamma A) are localized to the variable domain. We used RNase protection of this variable region to reveal the level of expression of gamma B and gamma C CaM kinase mRNAs in nine human tissues and cell lines. When transfected into Jurkat T cells, the gamma B cDNA encoded a functional kinase which cosedimented on sucrose gradients with endogenous T cell CaM kinase activity and formed a large multimeric enzyme. The recombinant gamma B isoform displayed two phases of autophosphorylation characteristic of CaM kinases, including the phase which converts it to a partially Ca(2+)-independent species. Site-directed mutagenesis of the predicted autoinhibitory domain yielded a mutant which was approximately 37% active in the absence of Ca2+/calmodulin, confirming the region as critical for autoregulation, and suggesting this mutant as a tool for studying the role of CaM kinase in nonneuronal tissues.
1992
Antisense Oligodeoxynucleotides to the Cystic Fibrosis Transmembrane Conductance Regulator Inhibit cAMP-activated but not Calcium-activated Chloride Currents.
Wagner JA, McDonald TV, Nghiem P, Lowe AW, Schulman H
Proc Natl Acad Sci U S A. 1992 Aug 1;89(15):6785-9.
PMID: 1379720
Abstract and Highlights
- Phosphorylation of the cystic fibrosis transmembrane conductance regulator (CFTR) by cAMP-dependent protein kinase leads to chloride flux in epithelial cells. Is CFTR also required for the calcium-dependent activation of chloride channels? We used antisense oligodeoxynucleotides to CFTR to reduce the expression of CFTR in colonic and tracheal epithelial cells. The antisense oligomers were a pair of adjacent 18-mers complementary to nucleotides 1-18 and 19-36 of CFTR mRNA. Sense and misantisense oligomers served as controls. A 48-h antisense treatment reduced the expression of CFTR protein as assayed by immunoprecipitation and autoradiography to 26% of the level in sense-treated T84 cells. Whole-cell patch clamp revealed that a 48-h antisense treatment of T84 and 56FHTE-8o- fetal tracheal epithelial cells reduced the cAMP-activated chloride current to approximately 10% of that in sense-treated cells. The half-life of functional CFTR is less than 24 h in these cells. In contrast, the calcium-activated chloride current was not affected by antisense treatment. Hence, the cAMP and calcium pathways are separate. CFTR is required for the cAMP pathway but not for the calcium pathway.
Human Lymphocytes Transcribe the Cystic Fibrosis Transmembrane Conductance Regulator Gene and Exhibit CF-defective cAMP-regulated Chloride Current.
McDonald TV, Nghiem P, Gardner P, Martens CL.
Send to J Biol Chem. 1992 Feb 15;267(5):3242-8.
PMID: 1371114
Abstract and Highlights
- Cystic fibrosis (CF) is the most common lethal genetic disease among Caucasians, primarily affecting epithelial tissues of the lung and gut. Mutations in a single gene, the cystic fibrosis transmembrane conductance regulator (CFTR), are responsible for this disease. Whether a physiological defect exists in the immune system of CF patients has remained controversial. A chloride ion transport defect has been described in human CF-derived lymphocytes; however, it has not been possible to detect CFTR mRNA in lymphocytes. We report here that normal human B-lymphoblasts display whole cell Cl- conductances induced by calcium-mediated pathways, volume regulation, and cAMP which are equivalent to currents described in epithelial cells. B-lymphoblasts from CF-affected humans demonstrated defective Cl- conductance regulation by cAMP but preserved regulation by calcium-mediated and volume regulation mechanisms. CFTR involvement in cAMP regulation of Cl- conductance in lymphocytes is further supported by our demonstration of the presence of appropriately spliced CFTR mRNA segments in human B and T lymphocytes as detected by an optimized reverse-transcription and polymerase chain reaction approach. The identity of the amplified products was confirmed by hybridization to CFTR-specific probes and DNA sequencing. Furthermore, the 3′-end of the gene was found in a T cell cDNA library. We conclude that CFTR mRNA is expressed in lymphocytes, consistent with the cAMP regulation of chloride transport present in normal lymphocytes but defective in CF-derived lymphocytes.
1991
Prostaglandin E1 Activates a Chloride Current in Jurkat T Lymphocytes via cAMP-Dependent Protein Kinase.
Maldonado D, Schumann M, Nghiem P, Dong Y, Gardner P.
FASEB J. 1991 Nov;5(14):2965-70.
PMID: 1721593
Abstract and Highlights
- Patch-clamp studies have identified a cAMP-dependent Cl- conductance in lymphocytes that is defectively regulated in cystic fibrosis. In this study we used 125I efflux and whole-cell patch-clamp studies to investigate whether prostaglandin E1 (PGE1), an agonist that generates intracellular cAMP in Jurkat T lymphocytes, activates a Cl- conductance. Stimulation of T cells by externally applied PGE1 stimulated 125I efflux and activated a slowly developing membrane current. When external and internal Cl- were about equal, the current reversed at about zero mV, but when external Cl- was lowered from 157 to 7 mM the reversal potential shifted 75 mV in the positive direction, demonstrating that the current carrier was Cl-. In addition, the current was blocked by 10 microM 5-nitro-2(3-phenylpropylamino) benzoic acid (NPPB), a potent Cl- channel blocker. A membrane-permeable cAMP analog mimicked the effect of PGE1, whereas intracellular application of a cAMP antagonist Rp-cAMP blocked the effect of PGE1. Addition of purified catalytic subunit of cAMP-dependent protein kinase (PKA) plus ATP to the recording pipette also activated a similar current, whereas internally applied Walsh inhibitor, the synthetic peptide inhibitor of PKA, blocked the PGE1 effect. These results suggest that PGE1, acting through PKA, activates a Cl- current in Jurkat T cells.